Can You Have H. Pylori and SIBO at the Same Time? Understanding Dual Infections
Can You Have H. Pylori and SIBO at the Same Time? Understanding Dual Infections
Digestive health issues can be complex and multifaceted, often leaving those affected searching for answers. Among the various digestive conditions that can occur simultaneously, the coexistence of Helicobacter pylori (H. pylori) and Small Intestinal Bacterial Overgrowth (SIBO) represents a particularly challenging scenario. This dual infection situation is more common than many realize and understanding the relationship between these two conditions is crucial for effective treatment and symptom management.
The Basics: Understanding H. Pylori and SIBO
Before diving into how these conditions can coexist, it's important to understand what each condition entails individually. Both conditions involve bacterial imbalances, but they affect different parts of the digestive system and manifest through various symptoms that can sometimes overlap.
What is H. Pylori?
Helicobacter pylori is a spiral-shaped bacterium that colonizes the stomach lining and the first part of the small intestine (duodenum). This resilient microorganism has evolved to survive the harsh acidic environment of the stomach by producing enzymes that neutralize stomach acid in its immediate vicinity. While many people with H. pylori remain asymptomatic, the infection can lead to chronic gastritis, peptic ulcers, and in some cases, increase the risk of gastric cancer.
H. pylori infection typically manifests with symptoms such as abdominal pain, bloating, nausea, frequent burping, and in more severe cases, unexplained weight loss. The bacterium's ability to alter stomach acid production can have far-reaching effects throughout the digestive system, potentially creating conditions favorable for other digestive disorders to develop.
What is SIBO?
Small Intestinal Bacterial Overgrowth occurs when there is an abnormal increase in the overall bacterial population in the small intestine, particularly types of bacteria not commonly found in that part of the digestive tract. The small intestine typically contains relatively few bacteria compared to the colon. When this balance is disrupted, and bacteria proliferate excessively, SIBO develops.
SIBO symptoms often include bloating, abdominal pain, diarrhea, constipation, excessive gas, and nutrient deficiencies. Many people with SIBO experience significant discomfort after consuming foods high in fermentable carbohydrates (FODMAPs), as these provide fuel for the overgrown bacteria, leading to fermentation and gas production in the small intestine.
The Connection Between H. Pylori and SIBO
The relationship between H. pylori and SIBO is complex and bidirectional. Research suggests that these conditions can influence each other's development and persistence through several mechanisms. Understanding these connections helps explain why treating one condition without addressing the other may lead to incomplete symptom relief.
How H. Pylori Can Lead to SIBO
H. pylori infection can create conditions that favor the development of SIBO through several pathways. First, by altering stomach acid production, H. pylori can reduce the acidic barrier that normally prevents excessive bacteria from entering the small intestine. Adequate stomach acid is our first line of defense against ingested pathogens, and when this acid barrier is compromised, bacteria can more easily colonize the small intestine.
Additionally, H. pylori infection can affect motility throughout the digestive tract. The migrating motor complex (MMC), which sweeps bacteria from the small intestine into the colon between meals, may become impaired due to inflammation and signaling disruptions caused by H. pylori. This reduced motility creates a more hospitable environment for bacterial overgrowth in the small intestine.
How SIBO Might Influence H. Pylori Infection
While less studied, there's evidence suggesting that SIBO might also influence H. pylori infection. The bacterial overgrowth in SIBO can lead to systemic inflammation and immune dysregulation, potentially affecting the body's ability to control H. pylori colonization. Furthermore, the altered intestinal environment in SIBO may impact the effectiveness of treatments aimed at eradicating H. pylori.
The dysbiosis (microbial imbalance) that occurs with SIBO can also disrupt the normal protective mechanisms of the gut microbiome, potentially allowing H. pylori to establish a stronger foothold or become more virulent. This creates a potential cycle where each condition reinforces the other, making treatment more challenging.
Recognizing Dual Infection: Symptoms and Diagnosis
Identifying when both conditions are present simultaneously can be challenging, as symptoms often overlap and one condition may mask or mimic the other. However, certain patterns and diagnostic approaches can help uncover the presence of both H. pylori and SIBO.
Overlapping Symptoms
When both H. pylori and SIBO are present, patients typically experience a more severe and persistent constellation of symptoms. These may include pronounced bloating, abdominal discomfort that varies in location and intensity, alternating bowel habits, early satiety, nausea, excessive gas, and nutrient malabsorption issues. Many patients report that their symptoms seem to worsen after meals, particularly those containing fermentable carbohydrates.
One distinctive feature of dual infection is the persistence of digestive symptoms despite successful treatment of one condition. For example, if H. pylori is eradicated but SIBO remains untreated, patients may experience initial improvement followed by a return of symptoms, often leading to frustration and continued health challenges.
Diagnostic Approaches
diagnosing both conditions requires a thoughtful and comprehensive approach. For H. pylori, testing options include breath tests, stool antigen tests, blood antibody tests, and endoscopic biopsies. For SIBO, hydrogen/methane breath testing remains the most accessible diagnostic tool, though some practitioners also use symptom assessment and empiric treatment trials.
When dual infection is suspected, it's generally recommended to test for both conditions, even if one has already been identified. This comprehensive approach helps ensure that treatment plans address all underlying issues rather than focusing on just one aspect of a more complex digestive problem.
Treatment Strategies for Dual Infections
Managing cases where both H. pylori and SIBO are present requires a strategic approach that addresses both conditions while supporting overall digestive health. Treatment success often depends on proper sequencing and comprehensive support throughout the healing process.
Sequential vs. Simultaneous Treatment
Clinicians often debate whether to treat these conditions simultaneously or sequentially. Many practitioners prefer to address H. pylori first, as its eradication may improve some of the conditions that contribute to SIBO. The standard treatment for H. pylori typically involves a combination of antibiotics and acid-suppressing medications for 10-14 days.
After H. pylori treatment, a follow-up test confirms eradication, followed by SIBO treatment if symptoms persist. SIBO treatment usually involves different antibiotics (such as rifaximin) or herbal antimicrobials, along with dietary modifications. This sequential approach helps clinicians assess the impact of each treatment and adjust strategies accordingly.
Supportive Measures and Digestive Enzymes
Beyond antimicrobial treatments, supporting overall digestive function is crucial for recovery and prevention of recurrence. Digestive enzymes can play a particularly important role in this process. Professional-grade enzyme complexes, such as Casa de Sante's low FODMAP certified digestive enzymes, provide comprehensive support for breaking down proteins, carbohydrates, and fats, which is especially beneficial when digestive function is compromised by infections.
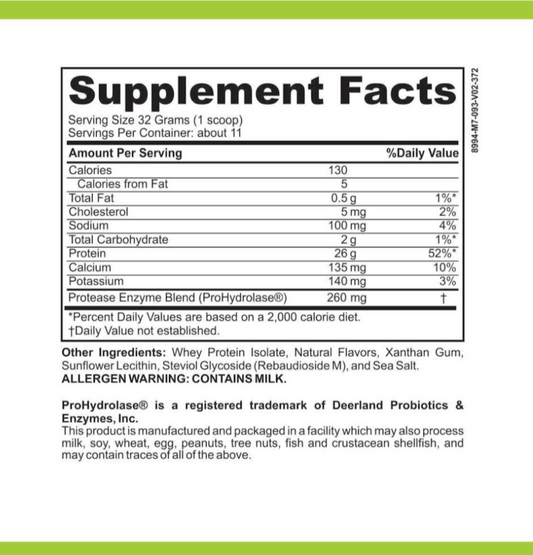
These specialized enzyme formulations contain targeted enzymes like protease complexes for protein digestion, amylase for carbohydrate breakdown, and lipase for fat digestion. For those dealing with the aftermath of H. pylori and SIBO, enzymes that support FODMAP digestion, such as alpha-galactosidase, can be particularly helpful in reducing symptoms while the digestive system heals. The comprehensive blend of 18 targeted enzymes in professional-grade formulations works synergistically to enhance nutrient absorption while reducing digestive stress during the recovery process.
Preventing Recurrence and Long-Term Management
Successfully treating dual infections is only part of the journey. preventing recurrence requires attention to the factors that may have contributed to the initial development of these conditions, along with ongoing support for optimal digestive function.
Dietary Considerations
Diet plays a crucial role in long-term management after treatment for H. pylori and SIBO. Many patients benefit from a phased dietary approach that begins with easily digestible foods and gradually reintroduces potential trigger foods. During this process, digestive enzyme supplements can be invaluable, helping to break down difficult-to-digest foods and enhance nutrient absorption.
For those with lingering sensitivity to FODMAPs after treatment, enzymes specifically designed to address these fermentable carbohydrates can make a significant difference in quality of life. Taking 1-2 capsules of a comprehensive enzyme formula at the beginning of each meal provides the digestive support needed during this critical healing phase and beyond.
Lifestyle Factors and Ongoing Support
Beyond diet, several lifestyle factors contribute to maintaining digestive health after treating dual infections. Stress management is particularly important, as chronic stress can alter motility and acid production, potentially creating conditions favorable for recurrence. Regular physical activity, adequate hydration, and mindful eating practices all support optimal digestive function.
For many individuals recovering from H. pylori and SIBO, continuing with supportive supplements like professional-strength digestive enzymes provides an added layer of protection against symptom recurrence. These non-GMO, third-party tested formulations offer peace of mind for those who have experienced the challenges of digestive infections and are committed to maintaining their newfound digestive freedom.
Conclusion
The coexistence of H. pylori and SIBO represents a significant challenge in digestive health, but with proper diagnosis and a comprehensive treatment approach, successful management is possible. Understanding the complex relationship between these conditions helps explain why addressing only one aspect of the problem often leads to incomplete resolution of symptoms.
For those navigating the complexities of dual infections, working with healthcare providers who recognize these connections is crucial. Additionally, supporting the digestive system with professional-grade enzyme supplements during and after treatment can make a meaningful difference in symptom management and quality of life. With the right approach, even those dealing with complicated digestive issues can experience the freedom of comfortable digestion and optimal nutrient absorption.