My IBS Is So Bad
My IBS Is So Bad
Living with irritable bowel syndrome (IBS) can be incredibly challenging. From the constant discomfort to the impact on daily life, this condition can have a significant effect on both physical and emotional well-being. In this article, we will explore the ins and outs of IBS, from its symptoms and severity to the available medical interventions and lifestyle changes that can help manage this condition effectively. We will also delve into coping mechanisms for IBS flare-ups and the importance of having a strong support system throughout this ongoing journey.
Understanding IBS: A Brief Overview
Irritable bowel syndrome, commonly referred to as IBS, is a chronic gastrointestinal disorder that affects the large intestine. It is characterized by abdominal pain, bloating, and changes in bowel habits, such as diarrhea or constipation. While the exact cause of IBS remains unknown, it is believed to be a result of a combination of factors, including abnormal gut contractions, increased sensitivity to pain, and disturbances in the gut-brain axis.
IBS is a complex condition that can have a significant impact on an individual's daily life. To better understand this condition, let's delve into its various aspects.
What is Irritable Bowel Syndrome?
IBS is a functional disorder, meaning that it does not cause structural abnormalities in the digestive system. However, its symptoms can be debilitating and significantly impact an individual's quality of life. The exact mechanisms behind IBS are not fully understood, but researchers believe that a combination of factors contribute to its development.
One possible factor is abnormal gut contractions. In individuals with IBS, the muscles in the intestines may contract too forcefully or too weakly, leading to changes in bowel habits. These abnormal contractions can result in diarrhea or constipation, depending on the specific subtype of IBS.
Another factor is increased sensitivity to pain. People with IBS often have a heightened sensitivity to pain in the gastrointestinal tract. This means that normal sensations, such as gas or stool passing through the intestines, can be perceived as painful or uncomfortable.
Disturbances in the gut-brain axis, which is the bidirectional communication between the gut and the brain, also play a role in IBS. The gut and the brain are connected through a complex network of nerves, hormones, and neurotransmitters. Disruptions in this communication system can lead to alterations in gut motility, sensation, and immune function, contributing to the development of IBS symptoms.
Common Symptoms of IBS
The symptoms of IBS can vary from person to person, with some experiencing predominantly diarrhea, while others suffer from constipation. Common symptoms include:
- Abdominal pain or discomfort: This is one of the hallmark symptoms of IBS. The pain is often described as crampy and can range from mild to severe.
- Bloating: Many individuals with IBS experience bloating, which is the feeling of increased abdominal fullness or distention.
- Gas: Excessive gas production is a common symptom of IBS and can contribute to bloating and discomfort.
- Changes in bowel habits: IBS can cause alterations in bowel movements, leading to diarrhea, constipation, or a combination of both. These changes may occur over time or even within the same day.
- A sense of incomplete bowel movements: Some individuals with IBS may feel like they haven't fully emptied their bowels after a bowel movement.
It is important to note that the severity and frequency of symptoms may fluctuate over time. Certain factors, such as stress, certain foods, and hormonal changes, can trigger or worsen IBS symptoms. Identifying and managing these triggers can be an important part of managing the condition.
By understanding the various aspects of IBS, we can gain insight into this complex condition and work towards better management and treatment strategies. If you suspect that you may have IBS, it is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
The Severity of My IBS
Living with severe Irritable Bowel Syndrome (IBS) can be an immense challenge, as it can disrupt daily life and even impact emotional well-being. Individuals with severe IBS often find themselves constantly adapting their routines to accommodate their symptoms and may experience limitations in engaging in activities they once enjoyed.
IBS is a chronic gastrointestinal disorder that affects the large intestine. It is characterized by symptoms such as abdominal pain, bloating, gas, and irregular bowel movements. While the exact cause of IBS is unknown, it is believed to be a combination of factors, including abnormal muscle contractions in the intestines, increased sensitivity to pain, and changes in the gut microbiome.
How IBS Affects My Daily Life
The constant abdominal pain, unpredictable bowel movements, and associated discomfort can make it difficult to carry out everyday tasks. Individuals with severe IBS may have to plan their outings meticulously, ensuring that they have access to restrooms or making arrangements to avoid triggers that exacerbate their symptoms.
For example, someone with severe IBS may need to carefully select the foods they eat, avoiding certain trigger foods like spicy or fatty foods, caffeine, and alcohol. They may also need to manage their stress levels, as stress can often worsen IBS symptoms. This may involve practicing relaxation techniques, such as deep breathing exercises or meditation.
The fear of experiencing symptoms in public can lead to social isolation and anxiety, further adding to the burden of IBS. Simple activities like going to a restaurant or attending social gatherings can become sources of stress and anxiety for individuals with severe IBS.
The Emotional Impact of Living with IBS
Living with IBS can take a toll on emotional well-being. The unpredictable nature of the condition and the impact it has on daily life can lead to feelings of frustration, embarrassment, and even depression. It is vital for individuals with IBS to seek emotional support and develop coping mechanisms to manage the emotional challenges that can accompany this condition.
Support groups, therapy, and counseling can provide individuals with a safe space to share their experiences, learn from others, and gain valuable coping strategies. It is important for individuals with IBS to prioritize self-care and engage in activities that promote relaxation and stress reduction.
Additionally, maintaining a healthy lifestyle can play a significant role in managing IBS symptoms and improving overall well-being. Regular exercise, a balanced diet, and adequate sleep can help reduce the severity and frequency of symptoms, as well as improve mood and energy levels.
While living with severe IBS can be challenging, it is important to remember that there are various treatment options available, including medications, dietary changes, and alternative therapies. It is crucial for individuals with IBS to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs and helps them regain control over their lives.
Medical Interventions for IBS
Seeking professional help is crucial for managing IBS effectively. A healthcare provider experienced in treating IBS can help devise a personalized treatment plan to address specific symptoms and reduce their impact on daily life.
Seeking Professional Help
Visiting a healthcare provider who specializes in gastrointestinal disorders is the first step towards managing IBS. They will conduct a thorough medical history review, perform diagnostic tests if necessary, and work closely with the individual to create an individualized treatment plan. This plan may involve medication to alleviate symptoms or manage specific aspects of IBS, such as diarrhea or constipation.
During the medical history review, the healthcare provider will ask detailed questions about the individual's symptoms, their frequency, and severity. They may also inquire about any triggers or patterns that the individual has noticed. This comprehensive approach helps the healthcare provider gain a deeper understanding of the individual's unique experience with IBS and tailor the treatment plan accordingly.
If necessary, the healthcare provider may order diagnostic tests to rule out other potential causes of the symptoms. These tests may include blood tests, stool analysis, or imaging studies. By ruling out other conditions, the healthcare provider can confirm the diagnosis of IBS and ensure that the treatment plan is appropriate.
Medications and Their Effectiveness
Several medications are available to help manage the symptoms of IBS. These may include antispasmodics to reduce gut contractions and alleviate cramping, laxatives or fiber supplements to relieve constipation, and anti-diarrheal medications to control diarrhea. It is important to note that the effectiveness of medication can vary from person to person, and finding the right balance may require some trial and error under medical supervision.
Antispasmodics are commonly prescribed to individuals with IBS who experience abdominal pain and cramping. These medications work by relaxing the muscles in the gut, reducing spasms and improving overall comfort. However, it is important to consider potential side effects, such as drowsiness or dry mouth, which may vary depending on the specific medication prescribed.
In cases where constipation is a predominant symptom of IBS, laxatives or fiber supplements may be recommended. Laxatives help soften the stool and promote regular bowel movements, while fiber supplements add bulk to the stool, making it easier to pass. The healthcare provider will determine the most suitable option based on the individual's specific needs and medical history.
For individuals with IBS who experience frequent episodes of diarrhea, anti-diarrheal medications can be beneficial. These medications work by slowing down the movement of the gut, allowing for better water absorption and firmer stools. It is important to follow the healthcare provider's instructions and use these medications as directed to avoid potential complications.
In addition to medication, the healthcare provider may also recommend lifestyle modifications to manage IBS symptoms. These may include dietary changes, stress management techniques, and regular exercise. By addressing various aspects of the individual's lifestyle, the treatment plan aims to provide comprehensive support and improve overall well-being.
Lifestyle Changes to Manage IBS
Besides medical interventions, certain lifestyle changes can also play a significant role in managing IBS effectively.
Dietary Adjustments for IBS
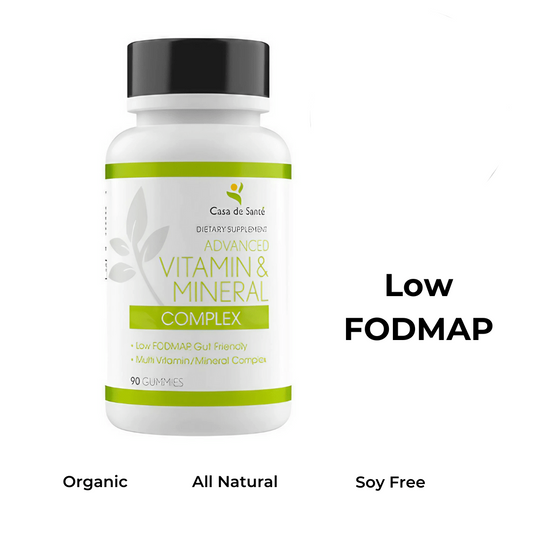
Adopting a low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet has shown positive results for many individuals with IBS. This diet involves reducing or eliminating foods that can trigger symptoms, such as certain fruits, vegetables, legumes, and grains. Keeping a food diary and working with a registered dietitian can help identify trigger foods and create a customized meal plan.
The Role of Exercise and Stress Management
Regular exercise can help alleviate symptoms associated with IBS. Engaging in activities such as yoga, walking, or swimming can improve digestion, reduce stress, and promote overall well-being. Stress management techniques, such as deep breathing exercises, mindfulness meditation, and therapy, can also be beneficial in managing IBS.
The Ongoing Journey with IBS
Over time, individuals with IBS develop coping mechanisms to navigate flare-ups and find ways to improve their overall well-being.
Coping Mechanisms for IBS Flare-ups
When experiencing a flare-up, individuals may find relief through techniques such as heat therapy, using hot water bottles or heating pads on their abdomen to alleviate cramping. Distraction techniques, such as engaging in hobbies or listening to calming music, can also help redirect focus away from the pain and discomfort.
The Importance of Support Systems
Building a strong support system is crucial for individuals living with IBS. Friends, family, and support groups can provide understanding, empathy, and helpful advice. Connecting with others who are facing similar challenges can provide a sense of validation and reassurance, making the journey with IBS less isolating.
In conclusion, living with severe IBS can be incredibly challenging, as it affects both physical and emotional well-being. Understanding the condition, seeking professional help, and making lifestyle changes can greatly improve an individual's quality of life. While there is no cure for IBS, managing symptoms and developing coping mechanisms are key. With the right support and a proactive approach, individuals with IBS can gain control over their condition and lead fulfilling lives.