A Root Cause Medicine Protocol For Patients With Eosinophilic Esophagitis Testing Therapeutic Diet And Supportive Supplements
A Root Cause Medicine Protocol For Patients With Eosinophilic Esophagitis Testing Therapeutic Diet And Supportive Supplements
Eosinophilic Esophagitis (EoE) is an allergic inflammatory disease of the esophagus characterized by the accumulation of eosinophils in the esophageal tissue. Although the exact cause of EoE is unknown, it is believed to be triggered by a combination of genetic and environmental factors. Currently, there is no cure for EoE, but the symptoms can be managed effectively through a root cause medicine protocol that includes testing therapeutic diet and incorporating supportive supplements.
Understanding Eosinophilic Esophagitis: An Overview
Eosinophils are a type of white blood cell that plays a crucial role in the body's immune response. These specialized cells are normally found in low levels in the esophagus, but in the case of Eosinophilic Esophagitis (EoE), they become excessively activated and infiltrate the esophageal tissue, causing inflammation and damage. This condition can lead to a range of distressing symptoms that significantly impact a person's quality of life.
When eosinophils accumulate in the esophagus, they release pro-inflammatory mediators, which further contribute to the development of symptoms. The exact mechanism by which eosinophils contribute to esophagitis is still not fully understood, but ongoing research is shedding light on this complex process.
One of the key challenges in diagnosing EoE is that its symptoms can vary from person to person. Additionally, these symptoms can often mimic other conditions, such as gastroesophageal reflux disease (GERD). This similarity in symptoms can lead to misdiagnosis or delayed diagnosis, prolonging the suffering of individuals with EoE.
The Role of Eosinophils in Esophagitis
Understanding the role of eosinophils in esophagitis is essential to comprehend the underlying mechanisms of EoE. Eosinophils are not only involved in the immune response but also play a role in tissue repair and remodeling. In the case of EoE, however, their activation becomes dysregulated, leading to an excessive accumulation in the esophageal tissue.
As eosinophils infiltrate the esophagus, they release a variety of pro-inflammatory mediators, such as cytokines and chemokines, which attract other immune cells to the affected area. This immune response contributes to the inflammation and damage observed in EoE. Additionally, the activation of immune cells further amplifies the inflammatory cascade, perpetuating the cycle of tissue damage and symptom development.
Researchers are actively investigating the specific triggers that lead to eosinophil activation in EoE. It is believed that both genetic and environmental factors play a role in this process. Identifying these triggers is crucial for developing targeted therapies that can effectively manage the symptoms and improve the quality of life for individuals with EoE.
Symptoms and Diagnosis of Eosinophilic Esophagitis
Recognizing the symptoms of EoE is vital for early diagnosis and appropriate management. However, the symptoms can be diverse and may overlap with other gastrointestinal conditions, making diagnosis challenging.
Common symptoms of EoE include difficulty swallowing (dysphagia), chest pain, heartburn, vomiting, and food impaction. These symptoms can vary in severity and frequency, and they may also be influenced by factors such as the type of food ingested or the presence of other underlying conditions.
To diagnose EoE, healthcare professionals consider a combination of clinical symptoms, endoscopic findings, and biopsy results. During an endoscopy, a thin, flexible tube with a camera is inserted into the esophagus to examine the tissue. Biopsy samples are then taken from the esophageal lining to assess the presence of eosinophils and the extent of inflammation.
It is important to note that diagnosing EoE requires a multidisciplinary approach involving gastroenterologists, allergists, and pathologists. Collaboration among these specialists is crucial to ensure accurate diagnosis and to tailor treatment plans to the specific needs of each individual.
The Root Cause Medicine Approach to Eosinophilic Esophagitis
Root cause medicine focuses on identifying and addressing the underlying factors contributing to a particular condition. In the case of EoE, the goal is to identify triggers and implement targeted interventions to reduce inflammation and improve symptoms.
Eosinophilic Esophagitis (EoE) is a chronic inflammatory condition that affects the esophagus. It is characterized by an abnormal accumulation of eosinophils, a type of white blood cell, in the lining of the esophagus. This can lead to symptoms such as difficulty swallowing, chest pain, and food impaction. While the exact cause of EoE is not fully understood, it is believed to be a combination of genetic and environmental factors.
Principles of Root Cause Medicine
Root cause medicine takes into account the individual's unique genetic makeup, medical history, environmental exposures, and lifestyle factors when designing a treatment plan. It aims to address the root causes of a condition rather than solely managing symptoms.
When it comes to EoE, a root cause medicine approach recognizes that each person's experience with the condition is unique. Factors such as genetic predisposition, food allergies, and environmental triggers can all play a role in the development and progression of EoE. By considering these factors, root cause medicine practitioners aim to develop personalized treatment plans that target the underlying causes of the condition.
Applying Root Cause Medicine to Eosinophilic Esophagitis
In the context of EoE, a root cause medicine protocol involves a comprehensive assessment of dietary and environmental factors, along with personalized interventions to reduce triggers and promote healing. This approach considers the immune system, gut health, and overall wellness of the individual.
One of the key aspects of root cause medicine for EoE is identifying and eliminating trigger foods from the diet. Common trigger foods for EoE include dairy products, wheat, soy, eggs, and certain fruits and vegetables. By working with a healthcare provider or registered dietitian, individuals with EoE can create an elimination diet plan to identify and remove these trigger foods from their diet.
In addition to dietary changes, root cause medicine practitioners may also recommend lifestyle modifications to support healing and reduce inflammation. This can include stress management techniques, regular exercise, and optimizing sleep quality. By addressing these lifestyle factors, individuals with EoE can potentially reduce the frequency and severity of symptoms.
Furthermore, root cause medicine recognizes the importance of gut health in managing EoE. The gut microbiome, which consists of trillions of microorganisms living in the digestive tract, plays a crucial role in immune function and overall health. Imbalances in the gut microbiome have been linked to various inflammatory conditions, including EoE. Therefore, interventions such as probiotic supplementation and gut-healing protocols may be recommended to restore balance and promote healing in the digestive system.
Overall, the root cause medicine approach to Eosinophilic Esophagitis aims to provide a comprehensive and personalized treatment plan that addresses the underlying factors contributing to the condition. By identifying triggers, implementing targeted interventions, and promoting overall wellness, individuals with EoE can potentially experience improved symptom management and a better quality of life.
The Impact of Therapeutic Diet on Eosinophilic Esophagitis
A therapeutic diet plays a central role in managing EoE. By identifying and eliminating specific food triggers, symptoms can be greatly improved and inflammation reduced.
Dietary Changes and Their Effect on Eosinophilic Esophagitis
The success of a therapeutic diet in EoE management depends on identifying and eliminating foods that trigger eosinophilic inflammation. This is typically achieved through an elimination diet, where common allergenic foods are gradually reintroduced to identify triggers. Foods commonly associated with EoE include milk, eggs, wheat, soy, peanuts, shellfish, and tree nuts.
Eliminating these trigger foods can be challenging, as they are often staples in our everyday diet. However, the benefits of a therapeutic diet are well worth the effort. By removing these triggers, individuals with EoE can experience a significant reduction in symptoms such as difficulty swallowing, chest pain, and heartburn.
Moreover, dietary changes can have a profound effect on the overall quality of life for those with EoE. By eliminating trigger foods, individuals can regain control over their symptoms and enjoy a better quality of life. They can participate in social gatherings without the fear of experiencing an EoE flare-up and can enjoy meals without the constant worry of triggering an allergic reaction.
Implementing a Therapeutic Diet: Practical Tips
Implementing a therapeutic diet for EoE requires careful planning and monitoring. It is essential to work with a healthcare professional, such as a registered dietitian, who can guide and support the individual throughout the process. Meal planning, label reading, and incorporating nutrient-rich alternatives are key strategies in implementing a successful therapeutic diet.
Meal planning is crucial to ensure that individuals with EoE are getting all the necessary nutrients while avoiding trigger foods. This involves creating a well-balanced meal plan that includes a variety of fruits, vegetables, lean proteins, and whole grains. It is important to consider individual preferences and dietary restrictions when developing a meal plan to ensure compliance and satisfaction.
Label reading is another essential skill that individuals with EoE must develop. Many packaged foods contain hidden allergens or ingredients that may trigger an allergic reaction. By carefully reading labels and understanding food labeling regulations, individuals can make informed choices and avoid potential triggers.
Incorporating nutrient-rich alternatives is also crucial in a therapeutic diet for EoE. For example, individuals who are allergic to milk can opt for calcium-fortified plant-based milk alternatives or incorporate other calcium-rich foods such as leafy greens, tofu, and almonds. By finding suitable alternatives, individuals can still meet their nutritional needs while avoiding trigger foods.
It is important to note that implementing a therapeutic diet for EoE is not a one-size-fits-all approach. Each individual may have different trigger foods and dietary needs. Therefore, working closely with a healthcare professional is essential to tailor the diet to the individual's specific requirements.
In conclusion, a therapeutic diet is a powerful tool in managing EoE. By identifying and eliminating trigger foods, individuals can experience a significant reduction in symptoms and inflammation. Implementing a therapeutic diet requires careful planning, label reading, and incorporating nutrient-rich alternatives. Working with a healthcare professional is crucial to ensure the diet is tailored to the individual's needs. With the right approach, individuals with EoE can regain control over their symptoms and enjoy an improved quality of life.
The Role of Supportive Supplements in Managing Eosinophilic Esophagitis
In addition to dietary modifications, supportive supplements can play a valuable role in managing EoE, enhancing immune function, and reducing inflammation.
Key Supplements for Eosinophilic Esophagitis
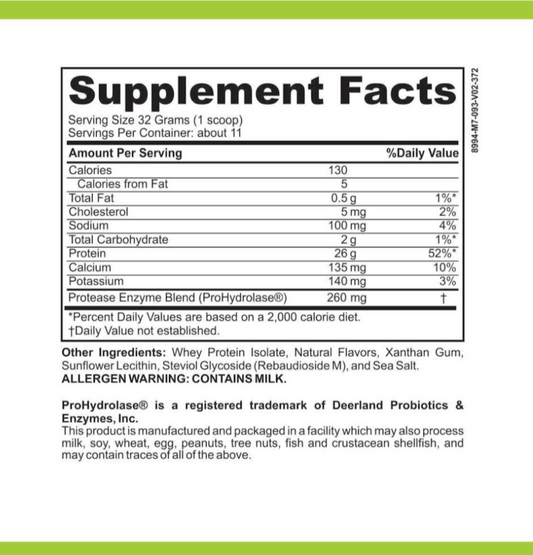
Several supplements have shown promise in EoE management. These include omega-3 fatty acids, vitamin D, probiotics, and digestive enzymes. These supplements can help modulate the immune response, promote gut health, and reduce inflammation in the esophagus.
How to Safely Incorporate Supplements into Your Treatment Plan
Supplement use should be discussed with a healthcare professional to ensure safety and effectiveness. Dosage, quality, and potential drug interactions should be taken into consideration. It is important to note that supplements should not replace a healthy diet but rather complement it in managing EoE.
Monitoring Progress and Adjusting the Protocol
Regular monitoring and assessment of symptoms and treatment response are crucial in managing EoE through a root cause medicine protocol.
Tracking Symptoms and Response to Treatment
Keeping a symptom diary or journal can help individuals and healthcare professionals track patterns and determine the effectiveness of the treatment plan. Tracking symptoms, dietary changes, and supplement intake can aid in adjusting the protocol as needed to optimize outcomes.
When and How to Modify the Root Cause Medicine Protocol
Modifications to the root cause medicine protocol may be necessary based on symptom severity, treatment response, and individual needs. Regular follow-up appointments with the healthcare professional can help guide these modifications and ensure that the protocol continues to address the root causes of EoE.
In conclusion, a root cause medicine protocol that includes testing therapeutic diet and incorporating supportive supplements can be an effective approach for managing EoE. By addressing the underlying factors contributing to the condition, symptoms can be reduced, and overall wellness can be improved. Working closely with healthcare professionals, individuals with EoE can take control of their condition and lead healthier lives.