Understanding IBS in Ashkenazi Jews
Understanding IBS in Ashkenazi Jews
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide. While it can affect individuals of any ethnic background, recent research has shown that certain populations may be more susceptible to developing IBS. One such population is Ashkenazi Jews, who have been found to have a higher prevalence of IBS compared to other ethnic groups. In this article, we will delve into the various aspects of IBS in Ashkenazi Jews, from understanding the condition itself to exploring its causes, diagnosis, treatment, and future implications.
What is IBS?
IBS, also known as spastic colon, is a chronic disorder that affects the large intestine (colon) and causes symptoms such as abdominal pain, cramping, bloating, gas, diarrhea, and constipation. While the exact cause of IBS remains unknown, it is believed to involve a combination of genetic, environmental, and psychological factors.
IBS is a common gastrointestinal condition that affects millions of people worldwide. It can have a significant impact on an individual's quality of life, causing discomfort and distress. The symptoms of IBS can vary in severity and frequency, with some individuals experiencing mild symptoms that are easily managed, while others may have more severe symptoms that significantly affect their daily activities.
Symptoms of IBS
The symptoms of IBS can vary from person to person, but they typically include abdominal pain or discomfort, changes in bowel habits (such as diarrhea, constipation, or both), bloating, excessive gas, and mucus in the stool. These symptoms can range from mild to severe, and they often come and go over time, making IBS a chronic condition.
The abdominal pain experienced by individuals with IBS can be crampy and may be relieved by passing gas or having a bowel movement. Some people may also notice that their symptoms worsen after eating certain foods or during times of increased stress. It is important to note that IBS does not cause any changes in the structure of the intestines or increase the risk of colorectal cancer.
Causes and Risk Factors of IBS
While the exact causes of IBS are still not fully understood, research suggests that certain factors may contribute to its development. These include abnormalities in the gut-brain axis, intestinal inflammation, altered gut microbiota, and heightened sensitivity to pain in the digestive system. Additionally, there is evidence to suggest that genetics and family history may play a role in predisposing individuals to IBS.
The gut-brain axis refers to the bidirectional communication between the gut and the brain. It involves the complex network of nerves and chemical messengers that regulate digestion and influence emotions and stress responses. In individuals with IBS, this communication system may be disrupted, leading to abnormal gut motility and sensitivity to pain.
Intestinal inflammation is another factor that has been implicated in the development of IBS. Studies have shown that individuals with IBS may have low-grade inflammation in their intestines, which could contribute to the symptoms experienced. The exact cause of this inflammation is not yet known, but it may be related to immune system dysfunction or alterations in the gut microbiota.
The gut microbiota refers to the community of microorganisms that reside in the intestines. These microorganisms play a crucial role in digestion and overall gut health. Research has shown that individuals with IBS may have an imbalance in their gut microbiota, with an overgrowth of certain bacteria or a decrease in beneficial bacteria. This dysbiosis may contribute to the symptoms of IBS and the inflammation observed in some cases.
Heightened sensitivity to pain in the digestive system is another factor that may contribute to the symptoms of IBS. Individuals with IBS may have a lower threshold for pain and may experience greater discomfort in response to normal bowel movements or distension of the intestines.
Diagnosis and Treatment of IBS
Diagnosing IBS can be challenging, as there are no specific tests or procedures that can definitively confirm the condition. Instead, doctors rely on the presence of consistent symptoms and the exclusion of other gastrointestinal disorders. It is important for individuals with symptoms of IBS to undergo a thorough medical evaluation to rule out other potential causes of their symptoms.
During the diagnostic process, doctors may perform various tests, such as blood tests, stool tests, and imaging studies, to rule out other conditions that may mimic the symptoms of IBS. In some cases, a colonoscopy or other endoscopic procedures may be recommended to visualize the intestines and rule out structural abnormalities.
Treatment for IBS typically focuses on managing symptoms and improving quality of life. This may involve dietary changes, stress management techniques, medications to alleviate symptoms, and psychological therapies such as cognitive-behavioral therapy. Dietary modifications may include avoiding trigger foods that worsen symptoms, increasing fiber intake, and incorporating probiotics into the diet to promote a healthy gut microbiota.
Stress management techniques, such as relaxation exercises, mindfulness meditation, and regular physical activity, can help individuals with IBS better cope with stress and reduce the frequency and severity of symptoms. Medications may be prescribed to relieve specific symptoms, such as antispasmodics for abdominal pain and cramping, laxatives for constipation, or anti-diarrheal agents for diarrhea.
Psychological therapies, such as cognitive-behavioral therapy, can be beneficial for individuals with IBS, especially those who have significant stress or anxiety related to their symptoms. These therapies can help individuals develop coping strategies, change negative thought patterns, and improve overall psychological well-being.
It is important for individuals with IBS to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific symptoms and needs. With proper management and lifestyle modifications, many individuals with IBS are able to effectively control their symptoms and lead fulfilling lives.
The Ashkenazi Jewish Population
The Ashkenazi Jewish population refers to Jews of Central and Eastern European descent. They represent the largest Jewish ethnic group worldwide and have a unique genetic profile due to centuries of isolation and genetic drift. Ashkenazi Jews have a higher prevalence of certain genetic disorders compared to other populations, which has led to extensive research into their genetic characteristics.
Brief History of Ashkenazi Jews
Ashkenazi Jews have a rich and complex history that spans centuries. Originating in the medieval Kingdom of Ashkenaz (which corresponds to modern-day Germany), they later migrated to various parts of Europe and formed distinct communities. Ashkenazi Jews have made significant contributions to various fields, including science, art, music, literature, and even culinary traditions.
Throughout their history, Ashkenazi Jews faced numerous challenges and experienced both periods of prosperity and persecution. In the Middle Ages, they were often subjected to discriminatory laws and restrictions, such as being confined to specific areas known as ghettos. Despite these hardships, Ashkenazi Jews managed to preserve their cultural identity and pass down their traditions from generation to generation.
During the Enlightenment period, Ashkenazi Jews began to experience greater integration into European society. Some Ashkenazi Jews became influential figures in academia and played key roles in the development of modern science and philosophy. Notable Ashkenazi Jewish thinkers include Moses Mendelssohn, who advocated for Jewish assimilation into German society, and Albert Einstein, whose groundbreaking theories revolutionized our understanding of the universe.
Genetic Characteristics of Ashkenazi Jews
Due to their unique genetic history and isolation, Ashkenazi Jews have a higher prevalence of certain genetic mutations compared to other populations. This includes mutations in genes associated with conditions such as Tay-Sachs disease, cystic fibrosis, Gaucher disease, and certain types of cancer.
The higher incidence of these genetic disorders among Ashkenazi Jews can be traced back to a phenomenon known as the "founder effect." During their migration and settlement in Eastern Europe, a small group of Ashkenazi Jews carried these genetic mutations. Over time, as the population grew, these mutations became more prevalent.
Despite the increased risk of certain genetic disorders, the genetic characteristics of Ashkenazi Jews have also provided valuable insights into human genetics and disease. Researchers have extensively studied the Ashkenazi Jewish population to identify specific genetic variants associated with various conditions. This knowledge has contributed to the development of genetic screening tests and targeted therapies for these disorders, benefiting not only Ashkenazi Jews but also other populations worldwide.
Furthermore, the genetic diversity within the Ashkenazi Jewish population has been a subject of scientific interest. Studies have revealed that Ashkenazi Jews share a common ancestry and have a relatively homogeneous genetic makeup. This genetic homogeneity has facilitated research on population genetics and the history of human migrations.
In conclusion, the Ashkenazi Jewish population's history and genetic characteristics are fascinating subjects of study. Their rich cultural heritage, resilience in the face of adversity, and significant contributions to various fields make them an integral part of the global community. The continued research into their genetic profile will undoubtedly lead to further discoveries and advancements in the field of genetics.
Prevalence of IBS in Ashkenazi Jews
While IBS affects individuals of all ethnic backgrounds, studies have shown that there is a higher prevalence of IBS among Ashkenazi Jews compared to other populations. This raises the question of whether there are specific genetic factors contributing to IBS in this ethnic group.
Studies on IBS in Ashkenazi Jews
Researchers have conducted several studies exploring the prevalence of IBS in Ashkenazi Jews and investigating potential contributing factors. One study found a higher prevalence of IBS in Ashkenazi Jews compared to Sephardic Jews and non-Jewish individuals. Another study suggested that genetic factors, such as mutations in certain genes associated with IBS, may contribute to the higher prevalence in this ethnic group.
Genetic Factors Contributing to IBS in Ashkenazi Jews
While the genetic factors contributing to IBS in Ashkenazi Jews are not yet fully understood, research has identified several genes that may play a role. These genes are involved in various biological processes, including inflammation, gut motility, and visceral hypersensitivity. Further research is needed to unravel the complex genetic mechanisms underlying IBS in this population.
Managing IBS in Ashkenazi Jews
Managing IBS in Ashkenazi Jews requires a comprehensive approach that takes into account the unique genetic and cultural characteristics of this population. While there is no cure for IBS, there are various strategies that can help alleviate symptoms and improve quality of life.
Dietary Considerations
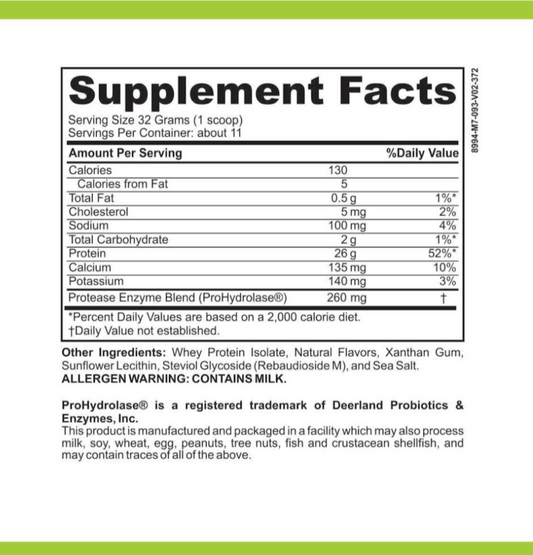
Diet plays a crucial role in managing IBS symptoms. Certain foods, such as those high in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), can trigger symptoms in individuals with IBS. Identifying and avoiding trigger foods can be beneficial. Additionally, incorporating fiber-rich foods, staying hydrated, and practicing portion control can also help manage symptoms.
Lifestyle Changes
In addition to dietary modifications, certain lifestyle changes can also make a difference in managing IBS symptoms. Regular exercise, stress management techniques (such as mindfulness meditation or yoga), and getting enough sleep can contribute to overall gut health and reduce the impact of stress on the digestive system.
Medical Interventions
In some cases, medical interventions may be necessary to manage IBS symptoms. This can include the use of medications to alleviate pain, regulate bowel movements, or manage specific symptoms such as diarrhea or constipation. It is important to work closely with healthcare professionals to determine the most appropriate treatment options.
Future Research and Implications
As research continues to shed light on IBS in Ashkenazi Jews, it opens up possibilities for future breakthroughs in diagnosis, treatment, and prevention of the condition. Ongoing studies are exploring the genetic basis of IBS and identifying potential targets for therapeutic interventions.
Ongoing Studies on IBS in Ashkenazi Jews
Several ongoing studies are focused on further understanding IBS in Ashkenazi Jews. These studies aim to identify additional genetic factors, explore the relationship between gut microbiota and IBS, and investigate potential biomarkers for diagnosing and monitoring the condition. The findings from these studies could pave the way for more personalized approaches to managing IBS in this specific population.
Potential Breakthroughs in IBS Treatment for Ashkenazi Jews
As our understanding of the genetic underpinnings of IBS in Ashkenazi Jews grows, it holds the promise of more targeted and effective treatments. By developing therapies that specifically address the genetic factors involved in IBS, we may be able to provide relief and improve the quality of life for individuals in this ethnic group.
In conclusion, understanding IBS in Ashkenazi Jews is a multi-faceted endeavor that encompasses various aspects of the condition, from its definition and symptoms to its prevalence, management, and future implications. While there is still much to learn, research is shedding light on the unique characteristics of IBS in this population, paving the way for improved diagnosis, treatment, and prevention strategies.