Functional GI Disorders
Functional GI Disorders
Functional GI disorders are a group of conditions that affect the normal functioning of the gastrointestinal (GI) tract. Unlike structural or organic GI disorders, functional GI disorders do not have a known physical cause. Instead, they are characterized by a combination of symptoms that can vary in intensity and duration. Despite their prevalence and impact on quality of life, functional GI disorders are often misunderstood and underdiagnosed. In this article, we will explore the definition, classification, symptoms, diagnosis, types, causes, and treatment of functional GI disorders.
Understanding Functional GI Disorders
Functional GI disorders are a group of conditions that are characterized by chronic or recurrent symptoms related to any part of the gastrointestinal (GI) tract. This includes the esophagus, stomach, small intestine, and colon. Unlike other GI disorders, functional GI disorders are not explained by structural or biochemical abnormalities. Instead, they are believed to be caused by abnormal sensory and motor functions of the GI tract.
One example of a functional GI disorder is irritable bowel syndrome (IBS). This condition is characterized by abdominal pain, bloating, and changes in bowel habits. Another example is functional dyspepsia, which is characterized by chronic or recurrent pain or discomfort in the upper abdomen. Functional constipation is also a common functional GI disorder, characterized by difficult or infrequent bowel movements.
Prevalence and Impact on Quality of Life
Functional GI disorders are surprisingly common, affecting a significant portion of the population worldwide. In fact, studies have shown that up to 25% of adults experience symptoms of a functional GI disorder at some point in their lives. This prevalence highlights the importance of understanding and addressing these conditions.
The impact of functional GI disorders on quality of life can be substantial. The chronic or recurrent nature of the symptoms can cause significant physical, emotional, and social distress. Individuals with functional GI disorders often experience pain, discomfort, and unpredictable bowel habits, which can interfere with daily activities and lead to a decreased overall sense of well-being.
Furthermore, the impact of functional GI disorders extends beyond the individual suffering from the condition. Work productivity may be affected, as individuals may need to take time off or experience decreased productivity due to their symptoms. Personal relationships may also be strained, as the symptoms can be embarrassing or disruptive to social activities.
It is important for individuals with functional GI disorders to seek proper diagnosis and management. With the right treatment plan, symptoms can be managed effectively, improving quality of life and allowing individuals to regain control over their daily activities and overall well-being.
Symptoms and Diagnosis of Functional GI Disorders
Common Symptoms
The symptoms of functional GI disorders can vary widely from person to person. However, some common symptoms include abdominal pain or discomfort, bloating, changes in bowel habits (such as diarrhea or constipation), indigestion, and nausea. These symptoms may occur in isolation or in combination, and their severity can range from mild to debilitating.
Abdominal pain or discomfort is a hallmark symptom of functional GI disorders. It can manifest as a dull ache, cramping, or sharp pain. The location of the pain can also vary, with some individuals experiencing it in the upper abdomen, while others feel it in the lower abdomen. The intensity of the pain can fluctuate throughout the day, and it may be triggered or worsened by certain foods or stress.
Bloating is another common symptom that individuals with functional GI disorders often experience. It is characterized by a feeling of fullness or tightness in the abdomen, as if it is distended. Bloating can be accompanied by excessive gas production, leading to burping or flatulence. This symptom can be particularly bothersome and can affect a person's quality of life.
Changes in bowel habits are also frequently reported by individuals with functional GI disorders. Some may experience diarrhea, which is characterized by loose, watery stools that occur more frequently than usual. Others may have constipation, where bowel movements become infrequent and difficult to pass. In some cases, individuals may alternate between episodes of diarrhea and constipation, further complicating their symptoms.
Indigestion, also known as dyspepsia, is a common symptom that can occur in functional GI disorders. It is characterized by a burning or discomfort in the upper abdomen, often accompanied by a feeling of fullness or early satiety. Indigestion can be triggered by certain foods, such as spicy or fatty meals, and it may worsen after eating.
Nausea is another symptom that individuals with functional GI disorders may experience. It is characterized by a sensation of queasiness or the urge to vomit. Nausea can be triggered by various factors, including certain foods, strong odors, or emotional stress. It can significantly impact a person's appetite and overall well-being.
Diagnostic Criteria and Procedures
Diagnosing functional GI disorders can be challenging due to the absence of clear physical markers or specific diagnostic tests. Instead, healthcare providers rely on a combination of clinical criteria and exclusion of other causes. The Rome criteria are widely used to establish a diagnosis, with specific criteria tailored to each functional GI disorder.
The Rome criteria provide guidelines for healthcare providers to assess the presence and severity of symptoms, as well as the duration and frequency of their occurrence. These criteria help differentiate functional GI disorders from other gastrointestinal conditions, such as inflammatory bowel disease or gastrointestinal infections.
In addition to the Rome criteria, healthcare providers may perform additional tests to rule out other conditions and provide a more accurate diagnosis. Blood tests can be used to assess for markers of inflammation or infection, as well as to evaluate liver and kidney function. Stool analysis may be conducted to check for the presence of blood, parasites, or bacterial overgrowth. Imaging studies, such as abdominal ultrasound or computed tomography (CT) scan, can provide detailed images of the gastrointestinal tract to identify any structural abnormalities. Endoscopic procedures, such as colonoscopy or upper endoscopy, may be performed to directly visualize the lining of the gastrointestinal tract and obtain tissue samples for further analysis.
It is important to note that the diagnostic process for functional GI disorders requires a comprehensive evaluation of the individual's medical history, physical examination, and symptom assessment. Healthcare providers take into consideration the patient's reported symptoms, their impact on daily life, and the exclusion of other potential causes before making a diagnosis.
Types of Functional GI Disorders
Functional gastrointestinal (GI) disorders are a group of conditions that affect the normal functioning of the digestive system. They are characterized by chronic or recurrent symptoms, such as abdominal pain, discomfort, and changes in bowel habits. Understanding the different types of functional GI disorders can help in the diagnosis and management of these conditions.
Irritable Bowel Syndrome (IBS)
IBS is one of the most common functional GI disorders, affecting millions of people worldwide. It is characterized by chronic or recurrent abdominal pain or discomfort, along with changes in bowel habits. These changes can include diarrhea, constipation, or a combination of both.
The exact cause of IBS is unknown, but it is thought to involve a complex interaction between genetic, environmental, and psychological factors. For example, certain genetic variations may increase the risk of developing IBS, while environmental factors such as infections or stressful life events can trigger symptoms.
IBS can be further classified into different subtypes, based on the predominant bowel pattern. These subtypes include:
- IBS with constipation (IBS-C): characterized by infrequent bowel movements and hard stools.
- IBS with diarrhea (IBS-D): characterized by frequent bowel movements and loose stools.
- IBS with mixed bowel habits (IBS-M): characterized by alternating episodes of constipation and diarrhea.
- Unsubtyped IBS (IBS-U): when the bowel pattern does not fit into any of the above subtypes.
Managing IBS involves a combination of lifestyle changes, dietary modifications, stress management, and medications. It is important for individuals with IBS to work closely with their healthcare providers to develop a personalized treatment plan.
Functional Dyspepsia
Functional dyspepsia is another common functional GI disorder, characterized by chronic or recurrent pain or discomfort in the upper abdomen. The symptoms can be accompanied by early satiety (feeling full after eating a small amount), bloating, or excessive belching.
Functional dyspepsia can be further classified into different subtypes, based on the dominant symptom:
- Postprandial distress syndrome (PDS): characterized by symptoms that occur after eating, such as feeling overly full or experiencing bloating.
- Epigastric pain syndrome (EPS): characterized by pain or discomfort in the upper abdomen, often unrelated to meals.
The underlying mechanisms of functional dyspepsia are not fully understood, but several factors have been implicated. Abnormalities in gastric motility, which is the movement of food through the stomach, may contribute to the development of symptoms. Additionally, increased sensitivity to stomach distension and low-grade inflammation in the stomach lining may also play a role.
Treatment for functional dyspepsia focuses on managing symptoms and improving quality of life. This can involve lifestyle modifications, such as avoiding trigger foods or eating smaller, more frequent meals. Medications that help reduce stomach acid or improve gastric motility may also be prescribed.
Functional Constipation
Functional constipation is characterized by infrequent bowel movements, difficulty passing stools, and a sensation of incomplete evacuation. It can be accompanied by abdominal pain or discomfort.
The development of functional constipation involves a combination of factors. Dysfunction of colonic motility, which is the movement of stool through the colon, can contribute to the condition. Impaired rectal sensation, where the rectum does not properly sense the presence of stool, can also play a role. Lifestyle factors, such as inadequate physical activity, a low-fiber diet, or not drinking enough fluids, can further contribute to the development of functional constipation.
Treatment for functional constipation often involves lifestyle modifications and dietary changes. Increasing fiber intake, drinking plenty of fluids, and engaging in regular physical activity can help improve bowel movements. In some cases, medications that promote bowel motility or soften stools may be prescribed.
In conclusion, functional GI disorders encompass a range of conditions that affect the normal functioning of the digestive system. Understanding the different types, such as irritable bowel syndrome, functional dyspepsia, and functional constipation, can aid in the management and treatment of these conditions. It is important for individuals experiencing symptoms to seek medical advice and work with healthcare providers to develop an individualized treatment plan.
Causes and Risk Factors
Genetic Factors
Genetic factors may contribute to the development of functional GI disorders, although the specific genes involved are not yet fully understood. Studies have shown that certain genetic variations may increase the risk of developing IBS or functional dyspepsia. However, more research is needed to unravel the complex interactions between genes and environmental factors in the pathogenesis of these disorders.
Environmental Triggers
Environmental factors, such as infections, dietary factors, and stress, can trigger or exacerbate symptoms in individuals with functional GI disorders. Infections, particularly gastrointestinal infections, have been linked to the development of functional GI disorders, with symptoms persisting long after the infection has cleared. Certain dietary components, such as high-fat foods or fermentable carbohydrates, can also contribute to symptom flares. Psychological stress, including anxiety and depression, can affect GI function and increase symptom severity.
Psychological Factors
Psychological factors, such as stress, anxiety, and depression, are known to play a role in the development and maintenance of functional GI disorders. Chronic stress can disrupt the normal communication between the brain and the gut, leading to alterations in GI function. Similarly, anxiety and depression can exacerbate symptoms and decrease the threshold for symptom perception. Psychological therapies, such as cognitive-behavioral therapy, can be effective in managing functional GI disorders.
Treatment and Management of Functional GI Disorders
Dietary Modifications
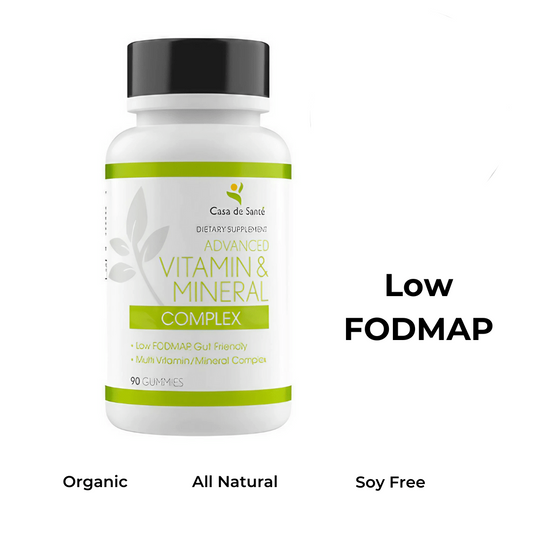
Dietary modifications are often recommended as an integral part of managing functional GI disorders. Strategies may include identifying and avoiding trigger foods, increasing fiber intake, and maintaining a balanced diet. Keeping a food diary and working with a registered dietitian can help identify individual triggers and develop a personalized dietary plan. In some cases, exclusion diets, such as a low FODMAP diet, may be recommended under the guidance of a healthcare provider.
Medication and Therapies
Medications may be used to manage specific symptoms associated with functional GI disorders. For example, antispasmodics or laxatives may be prescribed to alleviate abdominal pain or improve bowel function. Prokinetics, which enhance GI motility, can be beneficial for individuals with motility disorders. Additionally, certain antidepressant medications can help relieve symptoms by modulating pain perception and mood. Non-pharmacological therapies, such as acupuncture or hypnotherapy, may also be considered.
Lifestyle Changes and Stress Management
Lifestyle modifications and stress management techniques can complement other treatment approaches and improve overall well-being. Regular physical activity, adequate sleep, and stress reduction techniques, such as mindfulness or relaxation exercises, may help alleviate symptoms and decrease the frequency of flares. Psychological therapies, such as cognitive-behavioral therapy or gut-directed hypnotherapy, can be particularly effective for individuals with functional GI disorders associated with psychological factors.
In conclusion, functional GI disorders are common conditions that can significantly impact an individual's quality of life. While their exact causes remain elusive, a combination of genetic, environmental, and psychological factors likely contributes to their development. Diagnosis can be challenging due to the absence of definitive diagnostic tests, but healthcare providers use clinical criteria and exclusion of other causes to establish a diagnosis. Management typically involves a multifaceted approach, including dietary modifications, medications, and lifestyle changes. Psychological interventions can also play a crucial role in addressing the psychological factors associated with these disorders. Through a comprehensive and personalized approach, individuals with functional GI disorders can find relief and achieve a better quality of life.