Best Sugar Substitute For IBS
Best Sugar Substitute For IBS
Living with Irritable Bowel Syndrome (IBS) can be challenging, especially when it comes to identifying and avoiding trigger foods. For many people with IBS, sugar is one of the primary culprits that can worsen symptoms. Fortunately, there are several sugar substitutes available that can help satisfy your sweet tooth without causing digestive distress. In this article, we will explore the best sugar substitutes for IBS and discuss their benefits and drawbacks.
Understanding IBS: A Brief Overview
Before delving into the world of sugar substitutes, it is important to have a basic understanding of IBS. IBS, or Irritable Bowel Syndrome, is a common gastrointestinal disorder that affects the large intestine. It is characterized by recurring abdominal pain, bloating, gas, diarrhea, and/or constipation. While the exact cause of IBS is unknown, researchers believe that a combination of factors, including abnormal muscle contractions in the intestines, inflammation, and changes in the gut microbiota, play a role in its development.
IBS is a complex disorder that affects the function of the digestive system. It is a chronic condition that requires long-term management. People with IBS often experience a range of symptoms, including abdominal pain, changes in bowel patterns, and bloating. These symptoms can significantly impact their quality of life, making it important for individuals with IBS to find effective strategies to manage their symptoms and improve their overall well-being.
What is IBS?
IBS is a disorder that affects the normal functioning of the digestive system. It is considered a functional disorder, meaning that there are no structural abnormalities or visible signs of disease in the intestines of individuals with IBS. Instead, the symptoms experienced by those with IBS are thought to be a result of abnormal functioning of the gastrointestinal tract.
There are different subtypes of IBS, including IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), and mixed IBS (IBS-M), which involves both diarrhea and constipation. The symptoms experienced by individuals with IBS can vary in severity and frequency, with some people experiencing mild symptoms that are easily managed, while others may have more severe symptoms that significantly impact their daily lives.
Common Triggers of IBS
While specific triggers vary from person to person, there are certain foods and beverages that commonly contribute to IBS symptoms. It is important for individuals with IBS to identify their personal triggers in order to manage their symptoms effectively. Some of the most common triggers include:
- Fatty foods: Consuming high-fat foods, such as fried foods and fatty cuts of meat, can trigger symptoms in some individuals with IBS. These foods can be difficult to digest and may lead to increased bloating, gas, and abdominal discomfort.
- Caffeine: Beverages that contain caffeine, such as coffee, tea, and some sodas, can stimulate the digestive system and worsen symptoms in individuals with IBS. It is recommended to limit or avoid caffeine-containing drinks if they trigger symptoms.
- Alcohol: Alcoholic beverages can irritate the digestive system and lead to increased symptoms in individuals with IBS. It is advisable to moderate or avoid alcohol consumption to manage symptoms effectively.
- Spicy foods: Spices, such as chili peppers and hot sauces, can cause irritation in the gastrointestinal tract and trigger symptoms in some individuals with IBS. It may be beneficial to reduce or eliminate spicy foods from the diet to alleviate symptoms.
- Sugar: Sugar is another common trigger for individuals with IBS. Consuming excessive amounts of sugar, particularly in the form of sugary snacks, desserts, and beverages, can lead to increased gas, bloating, and diarrhea in some individuals. It is important to be mindful of sugar intake and consider alternative sweeteners if necessary.
It is worth noting that while these foods and beverages are commonly associated with triggering IBS symptoms, individual responses may vary. Some individuals with IBS may find that they can tolerate certain trigger foods in moderation, while others may need to avoid them completely. It is essential for individuals with IBS to work with a healthcare professional or registered dietitian to develop a personalized dietary plan that takes into account their specific triggers and nutritional needs.
The Role of Sugar in IBS
Sugar can be problematic for individuals with Irritable Bowel Syndrome (IBS) due to its impact on gut health. Consuming excessive amounts of sugar can disrupt the balance of gut bacteria and lead to increased inflammation in the digestive tract. This can result in worsened IBS symptoms.
How Sugar Affects IBS
When sugar is consumed, it is broken down into glucose and fructose. The fructose component can be difficult for some people with IBS to digest. Fructose malabsorption is a common issue among individuals with IBS, as their intestines have difficulty absorbing and processing this sugar. When undigested fructose reaches the colon, it can be fermented by gut bacteria, leading to gas, bloating, and diarrhea.
Furthermore, sugar can feed the pathogenic bacteria in the gut, leading to an overgrowth and further exacerbation of IBS symptoms. These bacteria produce gas and other byproducts that can irritate the intestinal lining, triggering symptoms such as abdominal pain and irregular bowel movements.
The Link Between Sugar and Digestive Health
Several studies have found a strong association between high sugar consumption and increased risk of digestive disorders, including IBS. Sugar has been shown to contribute to inflammation, gut permeability, and imbalances in gut bacteria.
Inflammation plays a crucial role in the development and progression of IBS. When the digestive tract is inflamed, it becomes more sensitive and reactive, leading to heightened symptoms. Sugar, particularly refined sugars found in processed foods and sugary beverages, can trigger an inflammatory response in the gut, worsening IBS symptoms.
Gut permeability, also known as "leaky gut," is a condition where the lining of the intestines becomes more permeable than normal. This allows toxins, bacteria, and undigested food particles to leak into the bloodstream, triggering an immune response and contributing to the development of IBS symptoms. Sugar has been shown to increase gut permeability, further compromising digestive health.
Moreover, imbalances in gut bacteria, known as dysbiosis, have been linked to various digestive disorders, including IBS. Sugar acts as a fuel source for pathogenic bacteria, allowing them to thrive and outnumber the beneficial bacteria in the gut. This imbalance can disrupt the delicate ecosystem of the gut microbiota, leading to gastrointestinal symptoms commonly experienced by individuals with IBS.
Given the negative impact of sugar on gut health, minimizing sugar intake is often recommended for individuals with IBS to help manage symptoms and promote gut health. This includes reducing the consumption of sugary snacks, desserts, sodas, and processed foods that are high in added sugars. Instead, opting for whole foods, such as fruits, vegetables, lean proteins, and whole grains, can provide essential nutrients while minimizing the detrimental effects of sugar on the digestive system.
Evaluating Different Sugar Substitutes
When searching for the best sugar substitute for IBS, it's essential to consider both artificial sweeteners and natural alternatives. Let's take a closer look at each category.
Artificial Sweeteners and IBS
Artificial sweeteners, such as aspartame and sucralose, are calorie-free alternatives to sugar. While these sweeteners can provide the sweetness you crave without the extra calories, they may not be suitable for everyone with IBS. Some people may experience digestive issues, such as bloating and gas, when consuming artificial sweeteners. It is best to test these sweeteners individually to determine how your body reacts.
Aspartame, one of the most commonly used artificial sweeteners, is found in a variety of sugar-free products, including diet sodas, chewing gum, and low-calorie desserts. It is approximately 200 times sweeter than sugar and has been approved by the U.S. Food and Drug Administration (FDA) for use in food and beverages. However, some individuals with IBS have reported experiencing gastrointestinal symptoms, such as diarrhea and abdominal pain, after consuming products containing aspartame.
Sucralose, another popular artificial sweetener, is commonly known by the brand name Splenda. It is made from sugar but undergoes a chemical process that replaces some of the sugar molecules with chlorine atoms, making it calorie-free. Sucralose is heat-stable, meaning it can be used in cooking and baking without losing its sweetness. While it is generally considered safe for consumption, some individuals with IBS have reported digestive discomfort, including bloating and gas, after consuming products containing sucralose.
Natural Sugar Substitutes and Their Impact on IBS
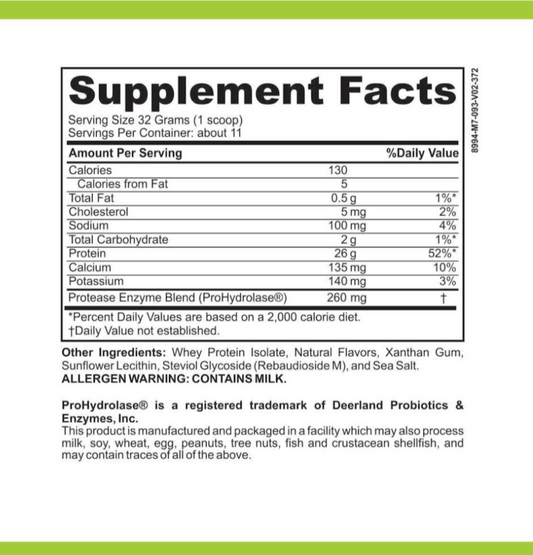
Alternatively, natural sugar substitutes can be a great option for individuals with IBS. These substitutes are derived from plants and offer a more natural alternative to refined sugar. Natural sweeteners like stevia, erythritol, and monk fruit sweetener have gained popularity for their minimal impact on blood sugar levels and digestive health.
Stevia, a plant native to South America, has been used for centuries as a sweetener and medicinal herb. It is derived from the leaves of the Stevia rebaudiana plant and is known for its intense sweetness. Stevia contains zero calories and does not raise blood sugar levels, making it suitable for individuals with IBS who are watching their sugar intake. Some studies have even suggested that stevia may have potential health benefits, such as anti-inflammatory and antioxidant properties.
Erythritol, a sugar alcohol, is naturally found in certain fruits and fermented foods. It has a sweet taste similar to sugar but contains fewer calories and has a minimal impact on blood sugar levels. Erythritol is not fully absorbed by the body, which means it passes through the digestive system without causing a significant increase in blood sugar or insulin levels. This makes it a suitable option for individuals with IBS who are looking for a sugar substitute that won't trigger digestive symptoms.
Monk fruit sweetener, also known as Luo Han Guo, is derived from the fruit of the Siraitia grosvenorii plant, native to southern China. It is a natural, zero-calorie sweetener that gets its sweetness from compounds called mogrosides. Monk fruit sweetener does not raise blood sugar levels and has been used in traditional Chinese medicine for its potential health benefits, including antioxidant and anti-inflammatory properties. While it may be more expensive than other sugar substitutes, it offers a natural and IBS-friendly alternative to refined sugar.
Top Sugar Substitutes for IBS
Stevia: A Natural Sweetener
Stevia is a plant-based sweetener that is extracted from the leaves of the Stevia rebaudiana plant. It is known for its intense sweetness without the calories or impact on blood sugar levels. Stevia is considered safe for individuals with IBS and can be used in various recipes and beverages.
Erythritol: A Sugar Alcohol
Erythritol is a sugar alcohol that occurs naturally in fruits and vegetables. It provides a sweet taste but is minimally absorbed by the body, resulting in low-calorie content. Erythritol is well-tolerated by most individuals with IBS and does not typically cause digestive issues. It can be used in baking and as a table sugar substitute.
Monk Fruit Sweetener: A Zero-Calorie Option
Monk fruit sweetener is derived from the monk fruit, a small melon-like fruit native to Southeast Asia. It contains natural compounds called mogrosides, which provide a sweet taste without the calories or impact on blood sugar levels. Monk fruit sweetener is safe for individuals with IBS and can be used in a variety of recipes.
Incorporating Sugar Substitutes into Your Diet
Tips for Using Sugar Substitutes
When incorporating sugar substitutes into your IBS-friendly diet, it's important to start slowly and monitor your body's response. Every individual is different, and what works for one person may not work for another. Experiment with different sugar substitutes, such as stevia, erythritol, or monk fruit sweetener, to find which one suits your taste preferences and digestion best.
Potential Side Effects of Sugar Substitutes
While sugar substitutes can be a helpful tool for managing IBS symptoms, it's important to be aware of potential side effects. Some people may experience mild digestive issues, such as bloating and diarrhea, when consuming sugar substitutes. If you notice any adverse reactions, discontinue use and consult with a healthcare professional.
Overall, finding the best sugar substitute for IBS requires individual experimentation. Stevia, erythritol, and monk fruit sweetener are all viable options that offer sweetness without the negative impact on gut health. By incorporating these sugar substitutes into your diet, you can satisfy your sweet cravings while managing your IBS symptoms effectively.