Low FODMAP Diet vs Low Glycemic Index Diet
Low FODMAP Diet vs Low Glycemic Index Diet
Understanding the Basics: What is a Low FODMAP Diet?
A low FODMAP diet is an eating plan that aims to reduce or eliminate certain carbohydrates known as FODMAPs from one's diet. FODMAPs, an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, are a group of sugars and sugar alcohols that are poorly absorbed in the small intestine. These undigested FODMAPs then travel to the large intestine, where they can be fermented by gut bacteria, leading to symptoms such as bloating, abdominal pain, and altered bowel movements in individuals with sensitive digestive systems.
The low FODMAP diet was developed by researchers at Monash University in Australia and has gained popularity in recent years as an effective approach for managing symptoms of irritable bowel syndrome (IBS) and other digestive disorders. By restricting high-FODMAP foods, individuals can potentially alleviate their digestive symptoms and improve their overall quality of life.
Understanding the Basics: What is a Low Glycemic Index Diet?
A low glycemic index (GI) diet focuses on consuming carbohydrates that have a low impact on blood sugar levels. The glycemic index is a measure that ranks foods based on how quickly they raise blood glucose levels after consumption. Foods with a high GI are rapidly digested and cause a sharp spike in blood sugar, while foods with a low GI are digested and absorbed more slowly, resulting in a gradual increase in blood sugar levels.
A low GI diet can be particularly beneficial for individuals with diabetes, as maintaining stable blood sugar levels is crucial for managing the condition. Additionally, this type of diet may also help with weight management, as foods with a low GI tend to provide a more sustained feeling of fullness and can prevent excessive hunger and cravings.
The Science Behind the Low FODMAP Diet
The low FODMAP diet is based on scientific research that has shown a strong association between FODMAP intake and the development of gastrointestinal symptoms in individuals with IBS. Studies have demonstrated that reducing FODMAP intake can significantly decrease symptoms such as bloating, gas, and abdominal pain in a substantial percentage of people with IBS.
The mechanism behind the effectiveness of the low FODMAP diet lies in the reduction of fermentable sugars and sugar alcohols that can lead to excessive gas production and water retention in the intestines. By limiting these substances, the diet aims to minimize their impact on the digestive system, resulting in symptom relief for many individuals.
The Science Behind the Low Glycemic Index Diet
The low glycemic index diet is supported by scientific evidence that demonstrates its positive effects on blood sugar control. Numerous studies have shown that consuming foods with a low GI can lead to better glycemic control, reduced insulin resistance, and improved lipid profile in individuals with diabetes.
Research has also suggested potential benefits of a low GI diet for weight management. Foods with a low GI tend to have a greater satiating effect, meaning they make individuals feel fuller for longer periods, reducing the likelihood of overeating and promoting weight loss.
Benefits of a Low FODMAP Diet
The low FODMAP diet offers several potential benefits for individuals struggling with digestive issues, especially those diagnosed with IBS. By effectively reducing or eliminating FODMAPs from the diet, many individuals experience significant relief from symptoms such as bloating, abdominal pain, constipation, and diarrhea. This can greatly improve their quality of life and allow them to engage in day-to-day activities without the constant discomfort and disruption caused by digestive issues.
Additionally, a low FODMAP diet may help identify specific food triggers for symptoms, allowing individuals to gain a better understanding of their unique dietary needs. With this knowledge, they can make more informed choices about the foods they consume and develop a personalized approach to managing their digestive health.
Benefits of a Low Glycemic Index Diet
The benefits of adhering to a low GI diet extend beyond glycemic control for individuals with diabetes. Maintaining stable blood sugar levels can help prevent energy crashes, manage hunger, and reduce the risk of developing complications associated with chronic high blood sugar levels. Furthermore, the gradual release of glucose from low GI foods ensures a sustained energy supply that can enhance physical performance and mental focus.
For individuals aiming to manage their weight, a low GI diet can be advantageous. Foods with a low GI are often rich in fiber and have a more substantial volume, which can promote feelings of fullness and prevent overeating. By maintaining a healthy weight, individuals can reduce their risk of various chronic conditions, including obesity, heart disease, and certain types of cancer.
Drawbacks and Challenges of a Low FODMAP Diet
While the low FODMAP diet has its benefits, it also poses some challenges and potential drawbacks. One major challenge is the restrictive nature of the diet. Many high-FODMAP foods are commonly consumed and may be staples in one's diet, such as wheat, garlic, onions, and certain fruits. Eliminating or significantly reducing these foods can make meal planning and eating out more difficult, as individuals must carefully scrutinize ingredient labels and discuss dietary restrictions with restaurant staff.
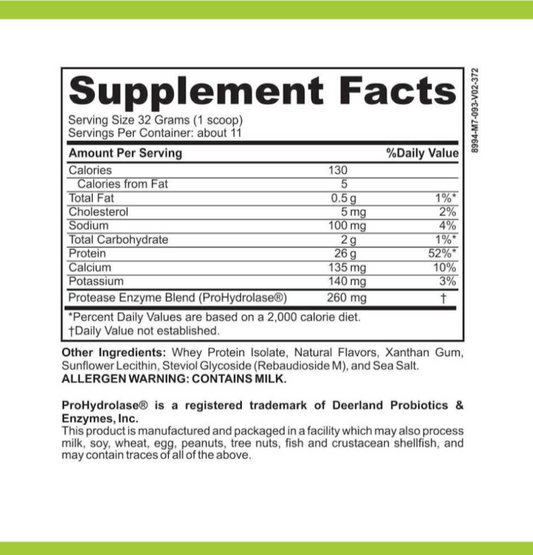
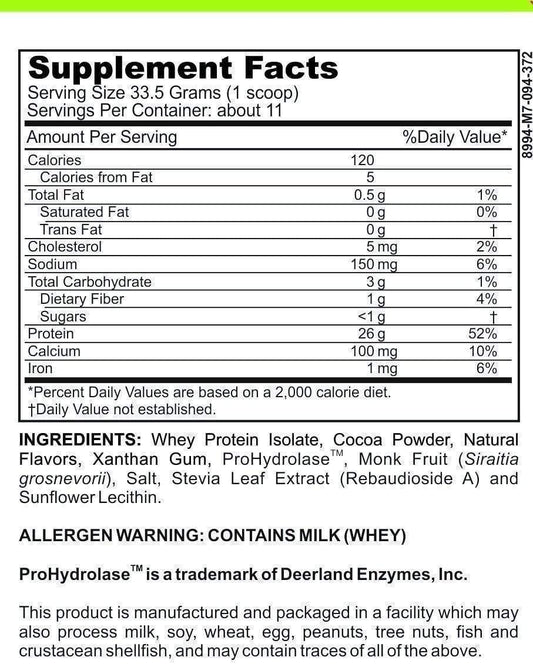
Another drawback of the low FODMAP diet is the potential for nutrient deficiencies. By excluding certain food groups, individuals may miss out on essential vitamins, minerals, and dietary fiber. Thus, it is crucial for individuals following this diet to work with a registered dietitian or nutritionist to ensure they are receiving adequate nutrition and to explore appropriate supplementation if needed.
Drawbacks and Challenges of a Low Glycemic Index Diet
Despite its benefits, a low GI diet also has its drawbacks and challenges. One challenge is that the glycemic index can vary depending on the preparation and combination of foods in a meal. It is not solely determined by the individual food item itself but can be influenced by various factors, such as cooking methods, ripeness, and other ingredients present in a meal. This can make it challenging to accurately predict the glycemic impact of a meal, especially when dining out or consuming complex meals.
Another difficulty faced by individuals following a low GI diet is the need for constant awareness and planning. It requires deliberate food choices, label reading, and meal preparation to ensure a consistently low GI intake. This level of attention and effort may not be feasible for everyone, especially those with limited time or resources for meal planning and preparation.
How to Implement a Low FODMAP Diet
If you are considering implementing a low FODMAP diet, it is essential to seek guidance from a registered dietitian who specializes in digestive health. They can provide detailed information on which foods to restrict and which to include, ensuring you are meeting your nutritional needs while effectively managing your symptoms. Additionally, working with a dietitian can help you overcome the challenges of avoiding high-FODMAP foods and adapting recipes to suit your dietary requirements.
Implementing a low FODMAP diet usually involves an initial elimination phase in which high-FODMAP foods are removed from the diet for a specified period, typically two to six weeks. This is followed by a reintroduction phase, during which individual FODMAP groups are gradually reintroduced to identify specific triggers and determine tolerance levels. Finally, a personalized FODMAP diet plan is created that allows for a varied and well-rounded diet while avoiding symptom-triggering foods.
How to Implement a Low Glycemic Index Diet
To implement a low GI diet, start by familiarizing yourself with the glycemic index values of different foods. Many resources, including online databases and smartphone applications, provide comprehensive lists and rankings of foods based on their GI values. Use these resources to guide your food choices and opt for foods that have a low or moderate GI value.
When planning meals, combine low GI foods with a source of protein and healthy fats to further slow down the digestion and absorption process. For example, pair whole grain carbohydrates with lean protein and incorporate sources of unsaturated fats, such as avocado or olive oil.
It is important to note that the GI value of a food can be influenced by various factors, including ripeness, cooking methods, and processing. For example, overripe fruit generally has a higher GI compared to the same fruit when it is at its peak ripeness. Additionally, cooking methods that break down starches, such as boiling, can increase the GI value of certain foods. Considering these factors and making informed choices can help optimize the benefits of a low GI diet.
Foods to Include in a Low FODMAP Diet
A low FODMAP diet typically encourages the consumption of foods that are naturally low in FODMAPs, allowing individuals to enjoy a varied and nutritious diet without triggering digestive symptoms. Foods that are generally safe to include on a low FODMAP diet include meat, fish, eggs, lactose-free dairy products, low FODMAP fruits and vegetables (such as berries, oranges, spinach, and zucchini), gluten-free grains (such as rice and quinoa), and certain nuts and seeds.
It is important to note that individual tolerances to FODMAPs can vary. Some individuals may find they can tolerate certain FODMAP-containing foods in smaller quantities or after specific preparation methods. Working with a dietitian can help you navigate these individual tolerances and create a personalized low FODMAP meal plan.
Foods to Include in a Low Glycemic Index Diet
A low GI diet emphasizes the consumption of foods that have a low or moderate GI value. This includes foods such as non-starchy vegetables (e.g., broccoli, leafy greens), legumes (e.g., lentils, chickpeas), whole grains (e.g., quinoa, oats), nuts and seeds, lean proteins (e.g., chicken, fish, tofu), and healthy fats (e.g., avocado, olive oil, nuts).
Adding fiber-rich foods to meals is also beneficial for maintaining a low GI diet. Fiber slows down digestion and helps regulate blood sugar levels. Thus, incorporating foods like chia seeds, flaxseeds, and psyllium husk can help optimize the glycemic impact of meals.
Foods to Avoid in a Low FODMAP Diet
A low FODMAP diet requires the avoidance or restriction of foods that are high in FODMAPs and can trigger symptoms. Common high-FODMAP foods include wheat and rye, onions and garlic, certain fruits (such as apples, pears, and stone fruits), lactose-containing dairy products, beans and legumes, certain sweeteners (such as honey, high fructose corn syrup), and some artificial sweeteners (such as sorbitol and xylitol).
It is important to note that not all foods from these categories contain high levels of FODMAPs. For example, some types of onions and garlic have lower FODMAP content and may be tolerated in limited quantities. Consulting a dietitian can help in identifying which specific foods to avoid and provide alternatives to ensure proper nutrition and variety in your diet.
Foods to Avoid in a Low Glycemic Index Diet
Avoiding high GI foods is the primary focus of a low GI diet. Foods to limit or avoid include refined grains (e.g., white bread, white rice), sugary snacks and desserts, sweetened beverages, and processed foods with added sugars. These foods are quickly digested and can cause rapid spikes in blood sugar levels.
It is also important to consider portion sizes when consuming moderate GI foods. While these foods have a lower impact on blood sugar levels compared to high-GI foods, consuming excessive quantities can still lead to elevated blood sugar levels. Monitoring portion sizes and pairing moderate GI foods with other low GI foods can help maintain stable blood sugar levels.
Meal Planning Tips for a Low FODMAP Diet
Meal planning on a low FODMAP diet can initially seem challenging, but with proper guidance and creativity, it becomes manageable. Consider the following tips when planning low FODMAP meals:
- Focus on naturally low FODMAP foods: Incorporate fruits, vegetables, meats, and grains that are naturally low in FODMAPs.
- Experiment with suitable alternatives: Explore alternative ingredients and preparation methods to recreate dishes that are typically high in FODMAPs. For example, use garlic-infused oil instead of garlic cloves for flavoring or opt for gluten-free bread instead of wheat-based bread.
- Read food labels: Be vigilant in reading ingredient labels to identify FODMAP-containing ingredients, such as high FODMAP sweeteners and additives.
- Plan meals in advance: Plan your meals and snacks ahead of time to ensure a balanced and varied low FODMAP diet.
- Seek professional guidance: Working with a registered dietitian who specializes in FODMAP diets can provide tailored recommendations and personalized meal plans to suit your individual needs.
Meal Planning Tips for a Low Glycemic Index Diet
To effectively plan meals that adhere to a low GI diet, keep the following tips in mind:
- Incorporate a variety of low GI foods: Aim to include a selection of non-starchy vegetables, whole grains, lean proteins, and healthy fats in each meal.
- Consider the glycemic load: In addition to the GI value, the glycemic load (GL) of a food takes into account the carbohydrate content in a typical serving size. Balancing both GI and GL can provide a more accurate reflection of a food's impact on blood sugar levels.
- Combine foods strategically: Pair low GI carbohydrates with proteins and healthy fats to further slow down digestion and promote satiety. For example, enjoy whole grain toast with scrambled eggs and avocado.
- Avoid overcooking starches: Overcooked or heavily processed starches tend to have a higher GI compared to less processed alternatives. Opt for cooking methods that preserve the natural structure of starch, such as steaming or lightly boiling.
- Prefer low GI snack options: Nuts, seeds, and fresh fruits make excellent low GI snacks when hunger strikes between meals.