Ulcerative Colitis: How Much Blood Is Too Much?
Ulcerative Colitis: How Much Blood Is Too Much?
Ulcerative colitis is a type of inflammatory bowel disease (IBD) that affects the lining of the colon and rectum. It is characterized by chronic inflammation and ulceration, which can lead to various symptoms, including abdominal pain, diarrhea, and rectal bleeding. In some cases, the bleeding associated with ulcerative colitis can be significant, causing concern for individuals living with this condition. Understanding the relationship between ulcerative colitis and blood loss is crucial for managing the disease effectively.
Understanding Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory bowel disease that affects the colon and rectum. It is classified as an autoimmune disease because the body's immune system mistakenly attacks the healthy cells in the colon and rectum. This immune response leads to inflammation and the formation of ulcers in the innermost lining of the large intestine.
The exact cause of ulcerative colitis is still unknown, but researchers believe that it is a combination of genetic and environmental factors. Some studies suggest that certain genes may make individuals more susceptible to developing the condition. Environmental factors such as diet, stress, and exposure to certain bacteria or viruses may also play a role in triggering the immune response.
Symptoms and Signs of Ulcerative Colitis
The symptoms of ulcerative colitis can vary from person to person and can range from mild to severe. Common signs and symptoms include:
- Persistent diarrhea: Individuals with ulcerative colitis often experience frequent and urgent bowel movements.
- Abdominal pain and cramping: The inflammation in the colon can cause discomfort and pain in the abdomen.
- Bloody stools: The ulcers in the colon can lead to rectal bleeding, resulting in the presence of blood in the stools.
- Rectal bleeding: This is a common symptom of ulcerative colitis and is often accompanied by bloody stools.
- Fatigue: Chronic inflammation and frequent bowel movements can lead to fatigue and a general feeling of weakness.
- Weight loss: Individuals with severe ulcerative colitis may experience weight loss due to a decreased appetite and nutrient malabsorption.
- Urgent need to have a bowel movement: The inflammation in the colon can cause a sudden and intense urge to have a bowel movement.
It is important to note that ulcerative colitis symptoms can come and go, with periods of remission and flare-ups. During remission, individuals may experience little to no symptoms, while flare-ups can be characterized by the worsening of symptoms and increased inflammation.
It is crucial for individuals experiencing these symptoms to seek medical attention for an accurate diagnosis and appropriate treatment. Ulcerative colitis can be managed with medications, lifestyle changes, and in severe cases, surgery may be necessary to remove the affected portion of the colon.
Living with ulcerative colitis can be challenging, but with proper medical care and support, individuals can lead fulfilling lives and effectively manage their symptoms.
The Link Between Ulcerative Colitis and Blood Loss
Why Does Ulcerative Colitis Cause Blood Loss?
The inflammation and ulceration that occur in ulcerative colitis can damage the blood vessels in the colon and rectum. This damage can lead to bleeding, resulting in blood in the stool or rectal bleeding. The inflammation also increases the production of mucus in the intestine, further contributing to the presence of blood in the stool.
When the immune system mistakenly attacks the lining of the colon and rectum, it triggers an inflammatory response. This inflammation causes the delicate blood vessels in the affected area to become swollen and fragile, making them more prone to rupture and bleed. The continuous damage to these blood vessels can result in chronic blood loss, leading to anemia and other complications.
Furthermore, the excessive production of mucus in the intestine, which is a characteristic feature of ulcerative colitis, can further exacerbate the blood loss. The mucus acts as a lubricant, facilitating the passage of stool. However, it can also contain blood, making the stool appear dark and tarry.
Normal vs. Abnormal Blood Loss in Ulcerative Colitis
While some degree of rectal bleeding is expected in individuals with active ulcerative colitis, it is essential to differentiate between normal and abnormal blood loss. Normal blood loss in this context refers to the typical bleeding associated with inflammation and ulceration in the colon. On the other hand, abnormal blood loss may involve more significant amounts of blood or persistent bleeding despite treatment.
Normal blood loss in ulcerative colitis is often characterized by intermittent episodes of mild to moderate rectal bleeding. This bleeding is usually self-limiting and resolves with appropriate medical management. It is important for individuals with ulcerative colitis to monitor their symptoms and report any changes in the pattern or severity of bleeding to their healthcare provider.
Abnormal blood loss, on the other hand, may indicate a more severe form of the disease or complications such as ulceration that extends deeper into the colon. In such cases, the bleeding may be more profuse, persistent, or accompanied by other symptoms such as abdominal pain, fatigue, or weight loss. Prompt medical attention is crucial to evaluate and address abnormal blood loss in ulcerative colitis to prevent further complications and ensure effective management.
Assessing Blood Loss in Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the large intestine and rectum. It can cause symptoms such as abdominal pain, diarrhea, and rectal bleeding. Monitoring and assessing blood loss are essential for individuals with ulcerative colitis to ensure timely intervention and management of the condition.
How to Monitor Blood Loss
Regular monitoring and assessment of blood loss play a crucial role in the management of ulcerative colitis. One common method includes observing changes in stool appearance. Individuals with ulcerative colitis often experience bloody stools or stools that appear dark and tarry. These visual cues can indicate the presence of blood and the severity of the bleeding.
In addition to visual observation, healthcare professionals may order blood tests to determine specific markers of blood loss. Hemoglobin levels, for example, can provide valuable information about the extent of the bleeding. Other blood markers, such as hematocrit and red blood cell count, can also be measured to assess the overall impact of blood loss on the body.
Furthermore, healthcare providers may use endoscopy, a procedure that involves inserting a flexible tube with a camera into the colon, to directly visualize the extent of inflammation and bleeding in the intestinal lining. This procedure allows for a more accurate assessment of blood loss and helps guide treatment decisions.
When to Seek Medical Attention
It is essential for individuals with ulcerative colitis to be vigilant about any changes in their symptoms, especially when it comes to rectal bleeding. If you notice an increase in the amount of blood in your stool, experience severe or persistent rectal bleeding, or have any concerns about your condition, it is crucial to seek medical attention promptly.
When you consult with your healthcare provider, they can evaluate the extent of the bleeding and determine the appropriate course of action to manage the situation effectively. They may recommend adjustments to your medication regimen, such as increasing the dosage or adding new medications to control inflammation and reduce bleeding.
In some cases, hospitalization may be necessary to provide more intensive treatment and close monitoring. This is particularly true if the bleeding is severe or if other complications, such as anemia or dehydration, have developed as a result of the blood loss.
Remember, early detection and intervention are key in managing ulcerative colitis and minimizing the impact of blood loss. By staying vigilant and seeking medical attention when needed, you can work with your healthcare team to develop an effective treatment plan and improve your quality of life.
Managing Ulcerative Colitis and Blood Loss
Ulcerative colitis is a chronic inflammatory bowel disease that affects the colon and rectum. It can cause symptoms such as abdominal pain, diarrhea, and rectal bleeding. One of the main goals in managing ulcerative colitis is to control inflammation and reduce symptoms, while also preventing complications like excessive blood loss.
Treatment Options for Ulcerative Colitis
When it comes to treating ulcerative colitis, there are several options available depending on the severity of the disease. Medications play a crucial role in managing the condition. Anti-inflammatory drugs, such as aminosalicylates, can help reduce inflammation in the colon and alleviate symptoms. Immunosuppressants, like azathioprine or methotrexate, may be prescribed to suppress the immune system and prevent inflammation. Biologic therapies, such as anti-TNF drugs, target specific proteins involved in the inflammatory process.
In some cases, when medication alone is not enough to control the disease, surgery may be necessary. Surgical intervention may involve removing the affected portion of the colon, which can provide long-term relief from symptoms and reduce the risk of complications. However, surgery is usually considered a last resort when other treatment options have been exhausted.
Lifestyle Changes to Minimize Blood Loss
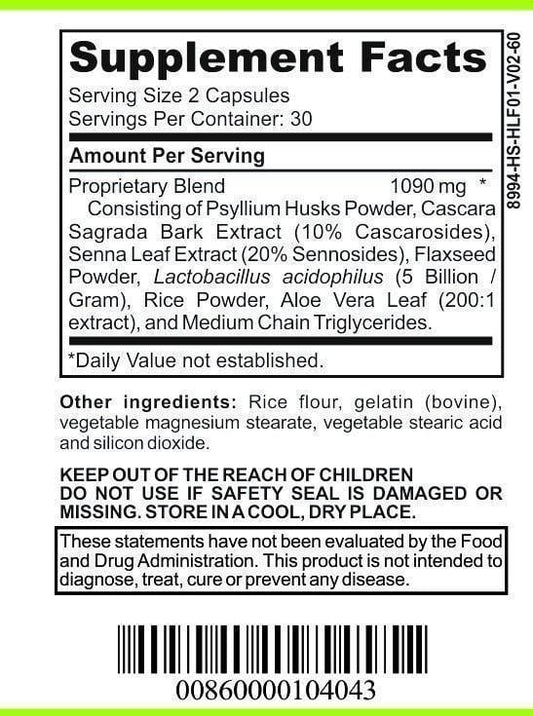
In addition to medical interventions, making certain lifestyle changes can help minimize blood loss in individuals with ulcerative colitis. One crucial aspect is following a balanced and nutritious diet. Consuming foods that are gentle on the digestive system, such as cooked vegetables, lean proteins, and easily digestible carbohydrates, can help reduce inflammation and promote healing.
Managing stress levels is also important, as stress can trigger flare-ups and worsen symptoms. Engaging in stress-reducing activities like yoga, meditation, or deep breathing exercises can help individuals with ulcerative colitis maintain a sense of calm and minimize the risk of blood loss.
Staying well-hydrated is another key factor in managing ulcerative colitis. Drinking plenty of fluids, especially water, can help prevent dehydration, which is common in individuals experiencing frequent diarrhea. Dehydration can exacerbate symptoms and increase the risk of blood loss, so it is essential to maintain proper hydration levels.
Avoiding triggers that can aggravate ulcerative colitis is also crucial. Alcohol, spicy foods, and high-fiber foods are known to cause flare-ups in some individuals. Identifying and avoiding these triggers can help minimize inflammation and reduce the risk of blood loss.
Engaging in regular exercise is beneficial for overall well-being and can also help manage ulcerative colitis. Physical activity can improve digestion, reduce inflammation, and promote a healthy immune system. However, it is important to consult with a healthcare professional before starting any exercise regimen, as certain activities may need to be modified based on individual circumstances.
Lastly, getting enough rest and sleep is essential for individuals with ulcerative colitis. Fatigue is a common symptom of the disease, and lack of sleep can exacerbate symptoms and increase the risk of blood loss. Prioritizing rest and establishing a regular sleep schedule can help manage fatigue and promote healing.
In conclusion, managing ulcerative colitis and minimizing blood loss involves a combination of medical interventions and lifestyle changes. By working closely with healthcare professionals, individuals with ulcerative colitis can find the most effective treatment options and make the necessary adjustments to their lifestyle to achieve optimal health and well-being.
The Long-Term Impact of Blood Loss in Ulcerative Colitis
Potential Complications and Risks
Chronic or excessive blood loss in ulcerative colitis can lead to anemia, a condition characterized by a low red blood cell count. Anemia can result in fatigue, weakness, shortness of breath, and other symptoms that can significantly impact quality of life.
Prognosis and Quality of Life
With appropriate management and treatment, many individuals with ulcerative colitis can lead normal lives. However, the presence of persistent or significant blood loss may increase the risk of complications and impact long-term prognosis. Regular monitoring, follow-up appointments with healthcare providers, and adherence to recommended treatments are crucial for maintaining a good quality of life.
In conclusion, while ulcerative colitis can cause blood loss, it is important to differentiate between normal and abnormal bleeding and seek timely medical attention when necessary. Effective management of ulcerative colitis, through a combination of medical interventions and lifestyle modifications, can help minimize blood loss and improve overall well-being for individuals living with this condition. Regular monitoring and follow-up care play essential roles in optimizing long-term outcomes and quality of life.