Semaglutide is a medication widely used for the treatment of type 2 diabetes and, more recently, for weight management. However, its gastrointestinal effects, particularly the occurrence of burps, can cause discomfort for many patients. This article explores various strategies to minimize the discomfort caused by semaglutide-induced burps, including dietary adjustments, lifestyle modifications, medical interventions, and ways to monitor and adjust treatment.
Key Takeaways
- Understanding the gastrointestinal side effects of semaglutide, such as burps, can help in developing effective coping strategies.
- Dietary adjustments, including avoiding certain foods and optimizing meal timing, can significantly reduce the frequency of semaglutide-related burps.
- Incorporating lifestyle changes, such as staying hydrated, engaging in regular physical activity, and managing stress, can alleviate burping and enhance overall well-being.
- Over-the-counter remedies may offer relief, but persistent symptoms should prompt consultation with a healthcare professional for personalized advice.
- Regularly monitoring symptoms and communicating with healthcare providers is crucial for adjusting semaglutide dosage and treatment to minimize side effects.
Understanding Semaglutide and Its Gastrointestinal Effects
The Mechanism of Semaglutide in the Body
Semaglutide operates by mimicking the GLP-1 hormone, which is naturally produced in the body. This hormone plays a crucial role in regulating blood glucose levels by stimulating insulin secretion and inhibiting glucagon release. Semaglutide's action helps to control blood sugar levels in individuals with type 2 diabetes.
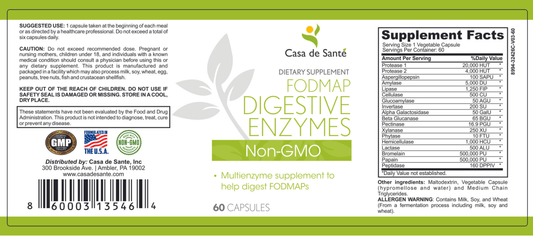
However, semaglutide can also affect the gastrointestinal system. It slows gastric emptying, which can lead to an increase in burping. This is where understanding the role of FODMAP digestive enzymes becomes essential. These enzymes are responsible for breaking down certain carbohydrates that can cause gas and bloating when not properly digested.
By managing the intake of high-FODMAP foods and supporting the body's digestive enzymes, patients may experience fewer semaglutide-induced burps.
It's important to monitor how your body responds to semaglutide and adjust your diet accordingly to minimize discomfort from burps.
Common Gastrointestinal Side Effects
Semaglutide, a medication used for the treatment of type 2 diabetes and obesity, is known to cause a range of gastrointestinal side effects. The most frequently reported issues include nausea, vomiting, diarrhea, constipation, and abdominal pain. These symptoms can vary in intensity and may affect daily activities and overall quality of life.
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Abdominal pain
While these side effects are generally manageable, they can sometimes lead to more serious complications if not addressed promptly. It is important for patients to monitor their symptoms and communicate any concerns with their healthcare provider.
Patients may also experience a feeling of fullness, reduced appetite, and changes in bowel habits. Understanding these side effects can help individuals anticipate and manage them more effectively, potentially reducing their impact on daily life.
Why Burps Occur with Semaglutide Use
Burps associated with semaglutide use are a result of its gastrointestinal effects. Semaglutide, a GLP-1 receptor agonist, slows gastric emptying, which can lead to an accumulation of gas in the stomach and subsequently, burping. This side effect is not uncommon and can be managed with certain strategies.
While not a direct cause, taking semaglutide alongside a multivitamin or other medications may influence the timing and frequency of burps due to interactions affecting digestion.
To minimize discomfort, consider the following:
- Monitoring the types of foods consumed
- Adjusting meal sizes and frequency
- Being mindful of the timing when taking semaglutide and multivitamins
Understanding these factors can help in reducing the frequency and intensity of burps, enhancing the overall treatment experience with semaglutide.
Dietary Adjustments to Alleviate Semaglutide-Related Burps
Foods to Avoid When Taking Semaglutide
When incorporating semaglutide into your treatment plan, it's crucial to consider the impact of certain foods on gastrointestinal symptoms, particularly burps. Avoiding high-fat meals and carbonated beverages can significantly reduce the frequency and intensity of burps.
- Fatty foods: These can slow stomach emptying, exacerbating burps.
- Carbonated drinks: The bubbles in these beverages can lead to gas and burping.
- Artificial sweeteners: Some sweeteners may cause bloating and increased gas.
- Dairy products: If lactose intolerant, these can contribute to gastrointestinal discomfort.
Adjusting your meal plans to exclude or limit these items can be an effective strategy in managing semaglutide-induced burps. It's also beneficial to eat smaller, more frequent meals rather than large ones, as this can help minimize digestive issues.
Remember, individual responses to foods can vary, so tracking your symptoms in relation to your diet can help identify personal triggers. Discussing these findings with a healthcare provider can lead to personalized meal plans that cater to your specific needs while on semaglutide therapy.
Recommended Dietary Practices
Adopting certain dietary practices can significantly reduce the occurrence of semaglutide-induced burps. Incorporate meals that are high in fiber and low in fat to promote digestive ease and minimize burping. Foods rich in complex carbohydrates, such as whole grains, legumes, and vegetables, are also beneficial as they are digested more slowly, reducing the likelihood of gas buildup.
- Eat smaller, more frequent meals throughout the day to avoid overloading the digestive system.
- Chew food thoroughly to aid in the breakdown of food and decrease air swallowing.
- Limit the intake of carbonated beverages and foods known to increase gas, such as beans, onions, and fried foods.
Maintaining a food diary can help identify specific foods that trigger burps, allowing for more personalized dietary adjustments. It's important to remember that dietary changes should be made gradually to allow the body to adapt.
Timing of Meals Relative to Semaglutide Dosage
The timing of meals in relation to semaglutide dosage can play a crucial role in managing gastrointestinal side effects, including burps. Adjusting meal schedules may help to minimize discomfort and enhance the medication's effectiveness.
- Eat a light meal or snack before taking semaglutide to reduce the likelihood of burps.
- Wait at least 30 minutes after dosing before consuming a large meal to allow the medication to be absorbed properly.
- Monitor your body's response to different meal timings and adjust accordingly.
By carefully observing how your body reacts to semaglutide at various times in relation to meals, you can identify the best eating schedule to mitigate burping and other gastrointestinal symptoms.
It's important to maintain a consistent routine once an optimal meal timing is established to ensure ongoing management of symptoms. Keep a diary of your meal times and symptom occurrence to discuss with your healthcare provider during your next visit.
Lifestyle Modifications for Managing Burps
Importance of Hydration
Maintaining adequate hydration is crucial when managing semaglutide-induced burps. Proper fluid intake can help facilitate digestion and reduce the occurrence of uncomfortable burping. It's important to drink water regularly throughout the day, rather than consuming large amounts at once, which can lead to bloating and exacerbate burping.
- Drink a glass of water before and after your semaglutide injection.
- Sip small amounts of water with meals.
- Avoid carbonated beverages as they can increase gas and burping.
Staying hydrated also helps to dilute stomach acids, which can become concentrated and lead to increased burping. By keeping the stomach environment balanced, you can minimize discomfort and improve overall digestive health.
Exercise and Physical Activity Considerations
Incorporating regular exercise into your routine can be beneficial for managing semaglutide-induced burps. Physical activity may help to improve gastrointestinal motility, which can reduce the frequency and intensity of burps. However, it's important to consider the type and timing of exercise to avoid exacerbating symptoms.
- Start with low-impact activities such as walking or yoga and gradually increase intensity.
- Avoid high-intensity workouts immediately after taking semaglutide, as they may increase burping.
- Schedule workouts a few hours after medication when the stomach has settled.
Inositol, a supplement sometimes recommended for various health issues, has not been directly linked to reducing semaglutide-related burps. However, maintaining a balanced diet that includes nutrients like inositol may contribute to overall digestive health. Consult with a healthcare professional before adding any supplements to your regimen.
While exercise is generally encouraged, it's crucial to listen to your body and adjust your activity level if you experience discomfort or an increase in burping.
Stress Management Techniques
Incorporating stress management techniques into your routine can be a pivotal step in managing semaglutide-induced burps. Mindfulness practices and relaxation exercises have been shown to reduce gastrointestinal discomfort by lowering stress levels, which can affect gut function.
Regular engagement in stress-reducing activities, such as yoga or meditation, can help alleviate the frequency and intensity of burps.
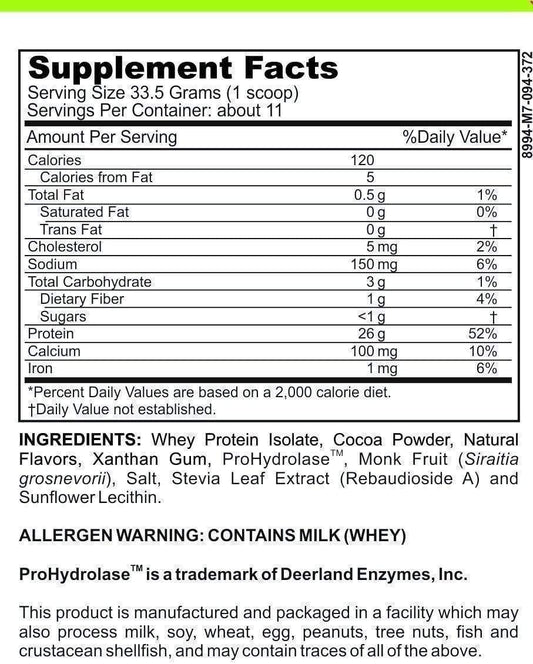
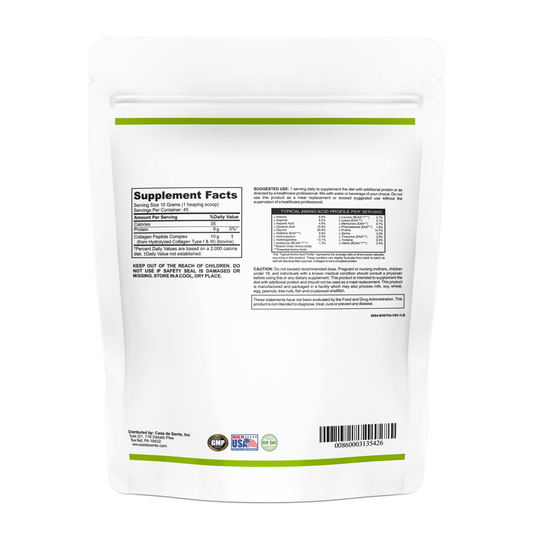
Additionally, certain dietary supplements, like a low FODMAP vanilla whey protein powder, may support digestive health while also providing a stress-relieving nutritional boost. Below is a list of simple stress management strategies to consider:
- Practice deep breathing exercises daily.
- Schedule time for activities that you enjoy and find relaxing.
- Ensure adequate sleep to help regulate stress hormones.
- Integrate a low FODMAP vanilla whey protein powder into your diet for its potential soothing effects on the digestive system.
Medical Interventions and Supportive Therapies
Over-the-Counter Remedies and Their Efficacy
When it comes to managing semaglutide-induced burps, patients often turn to over-the-counter remedies for relief. One such remedy that has gained attention is psyllium, a type of fiber that can aid in digestive health. Psyllium works by absorbing liquid in the intestines, which can help to stabilize the digestive process and potentially reduce the frequency of burps.
While not a cure-all, psyllium can be a valuable part of a broader strategy to manage gastrointestinal side effects associated with semaglutide.
It's important to note that the efficacy of psyllium and other over-the-counter remedies can vary from person to person. Here are some considerations for those looking to try psyllium:
- Start with a small dose to assess tolerance.
- Gradually increase the amount based on your body's response.
- Ensure adequate water intake to facilitate the fiber's action.
- Monitor for any changes in burping patterns or other gastrointestinal symptoms.
Patients should always consult with a healthcare professional before starting any new over-the-counter remedy to ensure it is appropriate for their individual health needs.
When to Consult a Healthcare Professional
While minor burps are a common side effect of semaglutide, persistent or severe symptoms warrant professional advice. Consult a healthcare provider if burps are accompanied by pain, significant discomfort, or if they persist despite self-management strategies.
- If burps significantly interfere with daily activities or sleep, seek medical attention.
- Unusual symptoms such as blood in vomit or severe abdominal pain are red flags.
- A healthcare professional can assess if symptoms are related to semaglutide or another condition.
It's crucial to differentiate between common side effects and potential complications that require medical intervention.
Support Groups and Counseling for Chronic Symptoms
For individuals experiencing persistent burps as a side effect of Semaglutide, support groups and counseling can provide much-needed relief and understanding. Engaging with others who face similar challenges offers emotional support and practical advice on managing symptoms.
- Support groups create a community of empathy and shared experiences.
- Counseling can help develop personalized strategies to cope with the discomfort.
- Both avenues can reduce feelings of isolation and improve overall well-being.
While medication and lifestyle changes are crucial, the psychological aspect of chronic symptoms should not be underestimated. Support groups and counseling address this by fostering a sense of community and resilience.
It's important to remember that chronic symptoms can impact more than just physical health; they can also affect mental and emotional well-being. Therefore, incorporating psychological support into the treatment plan can be a valuable component of comprehensive care.
Monitoring and Adjusting Semaglutide Treatment
Tracking Symptom Patterns and Triggers
Monitoring your body's response to Semaglutide is crucial in managing side effects such as burps. Keeping a detailed diary of your symptoms can reveal patterns and triggers, aiding in the identification of dietary or lifestyle factors that exacerbate discomfort. For instance, noting the onset of burps in relation to specific foods or stress levels can provide actionable insights.
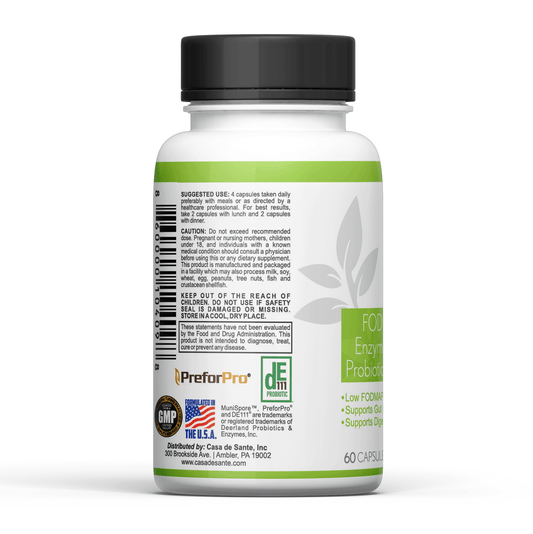
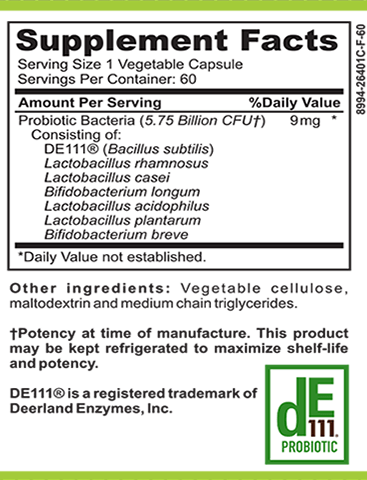
It's important to consider the role of diet in symptom management. Incorporating a low FODMAP probiotic and prebiotic regimen may help in balancing gut flora and reducing gastrointestinal disturbances.
Additionally, tracking the timing and frequency of burps can guide adjustments in meal planning and Semaglutide administration. Here's a simple framework to start with:
- Record the date and time of each burp episode.
- Note the severity and duration of the burps.
- List any foods consumed prior to the onset of symptoms.
- Include details about your stress levels and physical activity.
- Observe any changes when incorporating a low FODMAP probiotic and prebiotic into your diet.
By systematically documenting these factors, you can work with your healthcare provider to tailor your treatment plan for optimal comfort and efficacy.
Communicating with Your Healthcare Provider
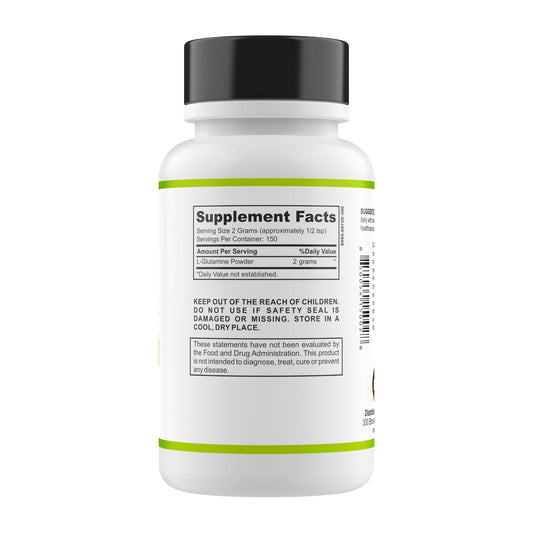
Effective communication with your healthcare provider is crucial when managing semaglutide-induced burps. Discussing the frequency and severity of your symptoms can lead to tailored advice and adjustments in your treatment plan. It's important to mention any supplements or medications you are taking, including glutamine, as they can interact with semaglutide.
Keeping a symptom diary can be beneficial. Note down the times when burps occur and any associated dietary or activity patterns. This information can help your healthcare provider understand the context of your symptoms and guide potential treatment modifications.
Remember to ask about:
- The possibility of adjusting your semaglutide dosage
- Alternative medications or supplements
- Non-pharmacological strategies to alleviate symptoms
Regular follow-ups ensure that any changes in your condition are monitored, and your treatment remains effective and safe.
Potential Adjustments in Dosage and Medication
When managing the side effects of Semaglutide, particularly burps, adjusting the dosage or medication itself may be necessary. This step should always be taken under the guidance of a healthcare provider. Patients may find that a lower dosage reduces symptoms, or that spacing out the dosage differently throughout the day provides relief.
- Discuss with your doctor the possibility of adjusting the dosage.
- Explore the timing of doses to see if symptoms improve with changes.
- Consider the use of complementary therapies, such as ashwagandha, which some patients report helps with gastrointestinal symptoms.
It's important to monitor your body's response to any changes in medication or dosage and report back to your healthcare provider. This collaborative approach ensures the best possible management of symptoms while maintaining the efficacy of the treatment.
Navigating the complexities of Semaglutide treatment requires careful monitoring and timely adjustments to ensure optimal outcomes. If you're seeking guidance on managing your treatment or exploring additional gut health solutions, visit our comprehensive resource hub. Our expertly curated content, including the FODMAP 101 Course and personalized meal plans, is designed to support your journey towards better health. Take the first step towards a more informed approach to your treatment by clicking on 'FODMAP 101 Course' today.
Conclusion
In summary, while semaglutide has emerged as a valuable medication in the management of conditions like diabetes and obesity, its side effects, such as burps, can be a source of discomfort for many patients. Throughout this article, we have explored a variety of strategies to mitigate these symptoms, from dietary adjustments to timing of medication intake. It's important for patients to consult with healthcare professionals to tailor these strategies to their individual needs. By taking a proactive approach and utilizing the tips provided, individuals can effectively manage semaglutide-induced burps and improve their overall treatment experience.
Frequently Asked Questions
What is Semaglutide and how does it affect the gastrointestinal system?
Semaglutide is a GLP-1 receptor agonist used primarily to treat type 2 diabetes and obesity. It mimics the hormone GLP-1 to stimulate insulin release and reduce appetite. Common gastrointestinal side effects include nausea, vomiting, diarrhea, and burps due to its effects on gastric emptying and digestive tract motility.
Why do burps occur with Semaglutide use?
Burps with Semaglutide use may occur because the medication slows gastric emptying, which can lead to a build-up of gas in the stomach and intestines. This excess gas is often released as burps.
What dietary changes can help reduce Semaglutide-induced burps?
To minimize burps, it's recommended to avoid gas-producing foods like beans, onions, and carbonated drinks. Eating smaller, more frequent meals and avoiding high-fat foods can also help. It's important to time meals appropriately in relation to Semaglutide dosage as advised by a healthcare provider.
Can lifestyle modifications alleviate the discomfort of Semaglutide-related burps?
Yes, lifestyle changes such as staying hydrated, engaging in regular physical activity, and managing stress can help reduce gastrointestinal discomfort, including burps. These practices support overall digestive health and can mitigate the side effects of Semaglutide.
Are there any over-the-counter remedies effective against Semaglutide-induced burps?
Some over-the-counter remedies like antacids or simethicone may provide temporary relief from burps. However, it's essential to consult a healthcare professional before using these remedies to ensure they're appropriate and won't interact with Semaglutide or other medications.
When should I consult a healthcare professional about Semaglutide-related burps?
If burps become frequent, severe, or are accompanied by other concerning symptoms such as abdominal pain or significant weight loss, it's important to consult a healthcare professional. They can assess whether the treatment needs to be adjusted or if additional interventions are necessary.