Is Dysbiosis The Same As Leaky Gut
In recent years, there has been a growing interest in the connection between our gut health and overall well-being. Two terms frequently discussed in this context are dysbiosis and leaky gut. While these conditions are often mentioned interchangeably, it is essential to understand that they are distinct entities with unique characteristics. In this article, we will take a closer look at both dysbiosis and leaky gut, exploring their definitions, causes, symptoms, and treatment options.
Understanding the Human Gut
Before delving into dysbiosis and leaky gut, it is crucial to gain a basic understanding of the human gut. The gut, also known as the gastrointestinal tract, plays a vital role in our overall health. It is responsible for digestion, absorption of nutrients, and immune function.
The human gut is a fascinating and complex organ system that spans from the mouth to the anus. It consists of various components, including the esophagus, stomach, small intestine, large intestine, and rectum. Each of these parts has a specific function in the digestive process.
Starting with the mouth, the process of digestion begins as soon as we take a bite of food. The teeth chew and break down the food into smaller pieces, while the saliva in our mouths helps to moisten and soften the food for easier swallowing. The food then travels down the esophagus, a muscular tube that connects the mouth to the stomach.
Once in the stomach, the food is mixed with gastric juices, including hydrochloric acid and enzymes, which help break down proteins and kill any harmful bacteria that may be present. The stomach's muscular walls contract and churn the food, further aiding in the digestion process.
From the stomach, the partially digested food enters the small intestine, where the majority of nutrient absorption takes place. The small intestine is lined with tiny finger-like projections called villi, which increase the surface area for nutrient absorption. Here, enzymes from the pancreas and bile from the liver help break down fats, proteins, and carbohydrates into smaller molecules that can be absorbed into the bloodstream.
After the small intestine, any undigested food particles, water, and electrolytes enter the large intestine, also known as the colon. The colon's main function is to absorb water and electrolytes, while also housing a diverse community of bacteria known as the gut microbiota.
The Role of Gut Flora
One of the key factors influencing gut health is the complex ecosystem of microorganisms residing within it. This community of bacteria, fungi, viruses, and other microscopic organisms is commonly referred to as gut flora or gut microbiota. These tiny residents support various functions such as synthesizing vitamins, breaking down undigested food particles, and maintaining a healthy immune system.
The gut microbiota is incredibly diverse, with trillions of microorganisms representing thousands of different species. Each person's gut microbiota is unique, influenced by factors such as genetics, diet, environment, and early life experiences. A healthy gut microbiota is characterized by a balance of beneficial bacteria, which promote good health, and potentially harmful bacteria, which can lead to various health issues.
Research has shown that disruptions in the gut microbiota, known as dysbiosis, can have significant implications for overall health. Dysbiosis can occur due to factors such as antibiotic use, poor diet, chronic stress, and certain medical conditions. When the balance of bacteria in the gut is disrupted, it can lead to digestive problems, inflammation, and a weakened immune system.
The Gut-Brain Connection
It is important to note that the gut is intricately connected to the brain through the gut-brain axis. This bidirectional communication system allows the gut to influence mental health and vice versa. The gut-brain axis plays a role in regulating stress responses, emotions, and cognitive function.
Within the gut, there is a vast network of neurons known as the enteric nervous system (ENS). The ENS is often referred to as the "second brain" due to its ability to function independently and communicate with the central nervous system (CNS). The ENS and CNS are connected via a complex network of nerves, hormones, and chemical messengers.
This gut-brain connection explains why individuals may experience gastrointestinal symptoms, such as stomachaches or diarrhea, during times of stress or anxiety. Similarly, digestive issues can also impact mental health, with studies linking gut dysbiosis to conditions like depression, anxiety, and even neurodegenerative disorders.
Understanding the intricate relationship between the gut and the brain is crucial for maintaining optimal health. By prioritizing gut health through a balanced diet, regular exercise, stress management, and probiotic-rich foods, individuals can support both their physical and mental well-being.
Defining Dysbiosis
Dysbiosis refers to an imbalance in the composition of the gut microbiota. In a healthy gut, there is a delicate balance between beneficial and potentially harmful microorganisms. The gut microbiota, also known as the gut flora, is a complex community of microorganisms that reside in the digestive tract. These microorganisms play a crucial role in maintaining overall health and well-being.
Within the gut microbiota, there are trillions of bacteria, viruses, fungi, and other microorganisms. These microorganisms interact with each other and with the host's body, influencing various physiological processes, including digestion, immune function, and metabolism. The balance of these microorganisms is essential for optimal gut health.
However, various factors can disturb this equilibrium, leading to dysbiosis. Dysbiosis can occur when there is an overgrowth of harmful bacteria or a decrease in beneficial ones. This imbalance can have significant implications for overall health and may contribute to the development of various health conditions.
Causes of Dysbiosis
Several factors can contribute to the development of dysbiosis. One of the most common causes is excessive antibiotic use. While antibiotics are essential for treating bacterial infections, they can also disrupt the delicate balance of the gut microbiota. Antibiotics not only kill the harmful bacteria causing the infection but also affect the beneficial bacteria in the gut, leading to dysbiosis.
Poor dietary choices can also play a role in dysbiosis. A diet high in processed foods, sugar, and unhealthy fats can promote the growth of harmful bacteria in the gut, while a diet rich in fiber, fruits, vegetables, and fermented foods can support a healthy gut microbiota.
Chronic stress is another factor that can contribute to dysbiosis. Stress can alter the gut-brain axis, a bidirectional communication system between the gut and the brain. This can lead to changes in gut motility, secretion of digestive enzymes, and the composition of the gut microbiota.
Certain medical conditions, such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and autoimmune disorders, can also disrupt the balance of the gut microbiota and contribute to dysbiosis. In these conditions, the immune system may be dysregulated, leading to inflammation in the gut and alterations in the gut microbiota.
Symptoms and Diagnosis of Dysbiosis
Dysbiosis can manifest with a range of symptoms, which can vary from person to person. Some common symptoms include bloating, gas, diarrhea, constipation, and abdominal discomfort. These symptoms can be quite distressing and can significantly impact a person's quality of life.
In addition to gastrointestinal symptoms, dysbiosis may also be associated with mental health issues such as anxiety and depression. The gut-brain axis plays a crucial role in the bidirectional communication between the gut and the brain. Disruptions in the gut microbiota can affect this communication, potentially contributing to the development or exacerbation of mental health conditions.
To diagnose dysbiosis, healthcare professionals may analyze stool samples to assess the composition of the gut microbiota. This analysis can provide valuable information about the types and abundance of microorganisms present in the gut. Additionally, other diagnostic tests, such as breath tests or blood tests, may be performed to further evaluate gut health and identify any underlying conditions that may be contributing to dysbiosis.
It is important to note that dysbiosis is a complex condition, and its diagnosis and treatment require a comprehensive approach. Healthcare professionals may recommend dietary modifications, probiotics, prebiotics, and other interventions to restore the balance of the gut microbiota and improve overall gut health.
Exploring Leaky Gut Syndrome
Leaky gut syndrome, also known as increased intestinal permeability, is a condition characterized by a disruption in the integrity of the intestinal lining. In a healthy gut, the intestinal barrier acts as a gatekeeper, allowing nutrients to pass through while keeping harmful substances out.
Causes of Leaky Gut
Various factors can contribute to the development of leaky gut syndrome. These include chronic inflammation, certain medications, excessive alcohol consumption, and gut infections. These factors can weaken the tight junctions between the intestinal cells, leading to increased permeability.
Symptoms and Diagnosis of Leaky Gut
Leaky gut syndrome may present with a diverse range of symptoms, including bloating, fatigue, food sensitivities, skin rashes, and joint pain. Since these symptoms can be nonspecific, diagnosing leaky gut requires a comprehensive evaluation, including a detailed medical history and specific laboratory tests.
Comparing Dysbiosis and Leaky Gut
While dysbiosis and leaky gut syndrome are distinct conditions, they can often coexist and influence each other. Understanding the similarities and differences between these two phenomena is essential for effective management and treatment.
Similarities Between Dysbiosis and Leaky Gut
Both dysbiosis and leaky gut have been associated with chronic inflammation, immune dysfunction, and various gastrointestinal symptoms. Moreover, the disruption of the gut-brain axis has been observed in both conditions, indicating potential links to mental health disorders.
Differences Between Dysbiosis and Leaky Gut
While dysbiosis primarily refers to an imbalance in the gut microbiota, leaky gut syndrome specifically denotes increased intestinal permeability. Dysbiosis can occur without increased permeability, whereas leaky gut always involves compromised intestinal integrity. It is important to note that addressing dysbiosis does not automatically resolve leaky gut, and vice versa.
Treatment Options for Dysbiosis and Leaky Gut
Managing dysbiosis and leaky gut involves a comprehensive approach that focuses on restoring gut health and optimizing overall well-being.
Dietary Changes and Supplements
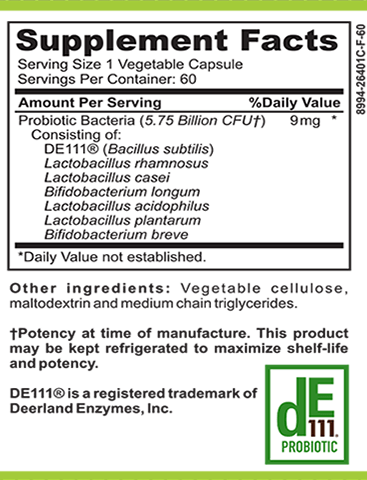
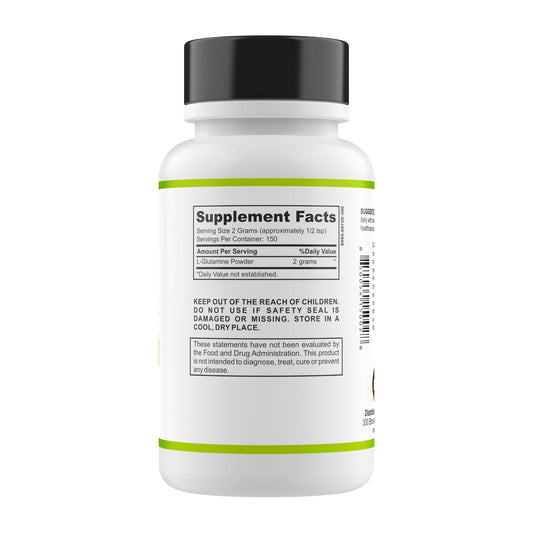
One of the key strategies to address dysbiosis and leaky gut is adopting a gut-friendly diet. This may involve reducing processed foods, refined sugars, and artificial additives while increasing the consumption of fiber-rich fruits, vegetables, and fermented foods. Probiotic and prebiotic supplements may also be recommended to support a healthy gut microbiota.
Medical Treatments and Therapies
In some cases, medical interventions may be necessary to manage dysbiosis and leaky gut. These may include targeted antimicrobial therapy to reduce harmful bacteria, anti-inflammatory medications to alleviate gut inflammation, and personalized treatment plans based on individual symptoms and underlying conditions. Additionally, stress management techniques and counseling may be beneficial in supporting the gut-brain axis.
In conclusion, while dysbiosis and leaky gut are often discussed together, it is important to recognize their distinct characteristics. Dysbiosis involves an imbalance in the gut microbiota, while leaky gut refers to increased intestinal permeability. These conditions can have overlapping symptoms and contribute to various health issues. By understanding the differences and similarities between dysbiosis and leaky gut, individuals can make informed decisions about their own gut health, seeking appropriate treatment options to regain balance and improve overall well-being.