How Long After Antibiotics Can I Take Probiotics
Antibiotics have become a staple in modern medicine, helping to combat bacterial infections and save countless lives. However, these powerful drugs can also disturb the delicate balance of bacteria in our bodies, particularly in the gut. With the increasing recognition of the importance of gut health, many people are turning to probiotics to restore their microbiome after a course of antibiotics. But how long should you wait after antibiotics before taking probiotics? Let's explore this topic further.
Understanding Antibiotics and Their Effects on the Body
Before we delve into the timing of probiotic intake, it's crucial to grasp the role antibiotics play in treating infections. These medications work by killing or inhibiting the growth of bacteria, effectively eradicating the targeted infection. However, in the process, antibiotics may also disturb the natural balance of bacteria in our bodies.
When antibiotics are prescribed for various infections, such as respiratory tract infections or urinary tract infections, they can be highly effective at eliminating harmful bacteria, reducing symptoms, and preventing the spread of infection. However, it's important to note that antibiotics are not selective in their action. While they target the infection-causing bacteria, they can also harm beneficial bacteria that help keep our bodies healthy.
The Role of Antibiotics in Treating Infections
Antibiotics are widely prescribed for their ability to combat infections. They are designed to specifically target and kill bacteria, either by directly killing them or by inhibiting their growth. This targeted approach helps to eradicate the infection and alleviate symptoms.
By eliminating the infection-causing bacteria, antibiotics prevent the infection from spreading to other parts of the body. This is particularly important in cases where the infection can lead to serious complications if left untreated.
However, the non-selective nature of antibiotics means that they can also affect the balance of bacteria in our bodies. While they target the harmful bacteria causing the infection, they can inadvertently harm the beneficial bacteria that play a crucial role in maintaining our overall health.
How Antibiotics Impact Your Gut Health
The gut, also known as the gastrointestinal tract, is home to trillions of bacteria collectively known as the gut microbiota. These bacteria play a vital role in various aspects of our health, including digestion, nutrient absorption, immune function, and overall well-being.
When antibiotics are taken, they can disrupt the delicate balance of the gut microbiota. The antibiotics not only target the harmful bacteria causing the infection but also affect the beneficial bacteria in the gut. This disruption can lead to an imbalance in the gut microbiota, which can have several consequences.
One of the most common consequences of antibiotic use is digestive issues. The disruption of the gut microbiota can result in symptoms such as diarrhea, bloating, and abdominal discomfort. These symptoms are often temporary and resolve once the gut microbiota regains its balance.
In some cases, however, the disruption of the gut microbiota can create an opportunity for opportunistic infections. Without the presence of beneficial bacteria to keep them in check, certain harmful bacteria or fungi may multiply and cause infections, such as Clostridium difficile infection or candidiasis.
Furthermore, the gut microbiota plays a crucial role in supporting our immune system. When the balance of the gut microbiota is disrupted by antibiotics, it can have a negative impact on immune function, potentially making us more susceptible to infections.
It's important to note that the impact of antibiotics on gut health can vary from person to person. Factors such as the type and duration of antibiotic use, individual gut microbiota composition, and overall health can influence the extent of the disruption and the subsequent effects on gut health.
The Importance of Probiotics for Gut Health
Probiotics are live microorganisms that can provide health benefits when consumed in adequate amounts. They have been extensively studied for their positive effects on gut health, including maintaining the balance of bacteria and supporting overall digestive function.
Gut health is crucial for maintaining overall well-being. The gut, also known as the gastrointestinal tract, is responsible for the digestion and absorption of nutrients from the food we consume. It is home to trillions of bacteria, both beneficial and harmful. When the balance of these bacteria is disrupted, it can lead to various digestive issues and even impact our immune system.
What are Probiotics?
Probiotics are typically found in fermented foods, such as yogurt, sauerkraut, and kefir. They can also be consumed in supplement form. These live microorganisms, such as Lactobacillus and Bifidobacterium strains, have been shown to promote a healthy gut by creating a favorable environment for beneficial bacteria to thrive.
When we consume probiotics, they can colonize the gut and compete with harmful bacteria for resources and space. This competition helps maintain a healthy balance of bacteria in the gut, preventing the overgrowth of harmful strains.
Benefits of Probiotics for Digestive System
Research has demonstrated that probiotics can aid in alleviating diarrhea, reducing symptoms of irritable bowel syndrome (IBS), and enhancing overall gut health. Probiotics can help restore the balance of bacteria in the gut, enhancing digestion and promoting regular bowel movements.
In addition to their impact on digestion, probiotics have also been found to support the immune system. The gut is closely linked to the immune system, and a healthy gut can help strengthen our body's defenses against infections and diseases.
Furthermore, probiotics have been studied for their potential role in reducing inflammation in the gut. Chronic inflammation in the gut can lead to various digestive disorders, such as Crohn's disease and ulcerative colitis. By modulating the immune response and reducing inflammation, probiotics may help manage these conditions and improve overall gut health.
It is important to note that the effectiveness of probiotics can vary depending on the specific strain and dosage. Different strains of probiotics may have different effects on gut health, and it is recommended to consult with a healthcare professional to determine the most suitable probiotic supplement or food source for individual needs.
In conclusion, probiotics play a crucial role in maintaining a healthy gut. They can help restore the balance of bacteria, enhance digestion, alleviate digestive issues, and support the immune system. Incorporating probiotic-rich foods or supplements into your diet can be a beneficial step towards improving gut health and overall well-being.
The Interaction Between Antibiotics and Probiotics
Given that antibiotics can disturb the gut microbiota, it may seem logical to begin taking probiotics immediately after completing an antibiotic course. However, the timing of probiotic intake can be influenced by various factors.
How Antibiotics Affect Probiotics
Antibiotics can potentially kill or suppress the growth of both harmful and beneficial bacteria in the gut. This means that taking probiotics while antibiotics are still actively fighting an infection may reduce their efficacy. Some of the live microorganisms in probiotic supplements might be destroyed by the antibiotics before they can colonize in the gut.
When antibiotics are administered, they target specific bacteria that are causing the infection. Unfortunately, they cannot differentiate between harmful and beneficial bacteria. As a result, the delicate balance of the gut microbiota can be disrupted. This disruption can lead to various gastrointestinal issues, such as diarrhea, constipation, or bloating.
Probiotics, on the other hand, are live microorganisms that can provide health benefits when consumed in adequate amounts. They are commonly found in fermented foods like yogurt, sauerkraut, and kimchi. By introducing these beneficial bacteria into the gut, probiotics aim to restore the natural balance of the microbiota.
The Need for Probiotics After Antibiotic Therapy
Despite the potential interaction between antibiotics and probiotics, research suggests that probiotic supplementation after antibiotic therapy can still provide benefits. Studies have indicated that probiotics can help restore the gut microbiota more rapidly and reduce the risk of antibiotic-associated diarrhea.
Antibiotic-associated diarrhea is a common side effect of antibiotic use. It occurs when the antibiotics disrupt the balance of the gut microbiota, allowing harmful bacteria like Clostridium difficile to flourish. Probiotics, by promoting the growth of beneficial bacteria, can help prevent this imbalance and reduce the risk of diarrhea.
Furthermore, probiotics have been shown to have immune-modulating effects. They can enhance the body's immune response and reduce inflammation in the gut. This can be particularly beneficial after a course of antibiotics, as the immune system may need support in rebuilding its defenses.
It is important to note that the effectiveness of probiotics may vary depending on the specific strains used and the individual's unique gut microbiota. Therefore, consulting with a healthcare professional is recommended to determine the most appropriate probiotic supplementation after antibiotic therapy.
In conclusion, while the interaction between antibiotics and probiotics is complex, there is evidence to suggest that probiotic supplementation after antibiotic therapy can provide benefits. By restoring the gut microbiota and supporting the immune system, probiotics can help mitigate the potential negative effects of antibiotics on the gastrointestinal system.
Timing the Intake of Probiotics After Antibiotics
When it comes to the timing of taking probiotics after antibiotics, there is no one-size-fits-all answer. However, there are some general guidelines that can help you make an informed decision.
It is widely recommended by experts to wait at least two hours after taking antibiotics before consuming probiotics. This interval allows the antibiotics to exert their therapeutic effect on the infection before introducing probiotics that may be susceptible to the antimicrobial properties of antibiotics.
However, it is important to note that the ideal timing of probiotic intake can be influenced by various factors. One such factor is the specific antibiotic that was used. Different antibiotics have different mechanisms of action and may persist in the body for varying lengths of time. Therefore, it is crucial to consider the specific antibiotic you have taken when determining the timing of probiotic intake.
Another factor to consider is the duration of antibiotic therapy. If you have been on a short course of antibiotics, waiting a couple of hours before starting probiotics may be sufficient. However, if you have undergone a prolonged antibiotic treatment, it may be advisable to wait a little longer before introducing probiotics to allow your body to recover and restore its natural balance.
Furthermore, individual factors such as overall health and susceptibility to gut disturbances can also play a role in determining the timing of probiotic intake. If you have a compromised immune system or a history of gastrointestinal issues, it may be wise to consult with a healthcare professional for personalized advice tailored to your unique situation.
In conclusion, while there are some general guidelines for timing the intake of probiotics after antibiotics, it is important to consider individual factors and seek professional advice when making decisions about your health. By taking these factors into account, you can ensure that you are giving your body the best chance to benefit from both antibiotics and probiotics.
Choosing the Right Probiotic Supplement After Antibiotics
Not all probiotic supplements are created equal, and selecting the right one is essential for reestablishing a healthy gut microbiota after antibiotics.
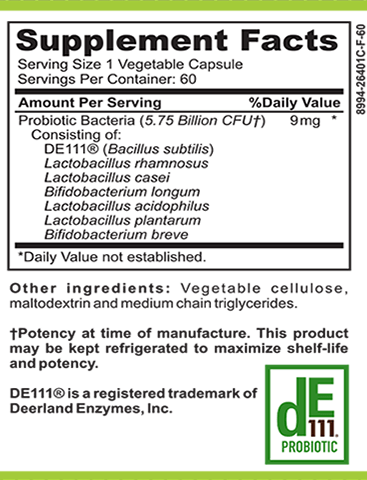
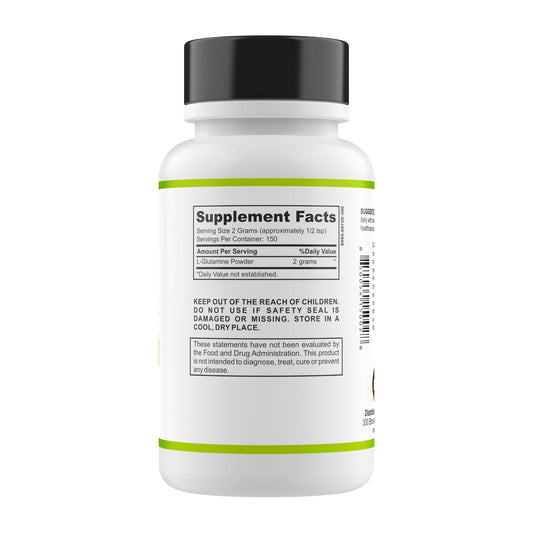
Types of Probiotics to Consider
Look for a probiotic supplement that contains well-studied strains, such as Lactobacillus acidophilus, Bifidobacterium lactis, or Saccharomyces boulardii. These strains have demonstrated positive effects on gut health in numerous studies.
Tips for Selecting a Quality Probiotic Supplement
When choosing a probiotic supplement, opt for products that have been tested for potency, stability, and safety. Look for products with a high number of colony-forming units (CFUs) and ensure that they are stored properly to maintain their efficacy.
In conclusion, while there is no set timeframe for taking probiotics after antibiotics, waiting a few hours after completing the antibiotic course before introducing probiotics may be beneficial. Ultimately, it is essential to consider individual factors and consult with a healthcare professional for personalized advice. By understanding the interaction between antibiotics and probiotics and making informed choices, you can support your gut health and promote a balanced microbiome for overall well-being.