How Having My Gallbladder Removed Affected My IBS
When I was diagnosed with irritable bowel syndrome (IBS), little did I know that my gallbladder would also play a significant role in my digestive journey. Understanding the function of the gallbladder and its connection to IBS has been crucial in managing my symptoms post-removal. In this article, I will share my personal experience and offer coping strategies for those facing similar challenges.
Understanding the Function of the Gallbladder
The gallbladder, a small pear-shaped organ located beneath the liver, plays a vital role in digestion. Its primary function is to store and concentrate bile, a substance produced by the liver, which aids in the breakdown and absorption of fats. When we consume a fatty meal, the gallbladder contracts, releasing bile into the small intestine to facilitate the digestion process.
The Gallbladder's Role in Digestion
Bile, produced by the liver and stored in the gallbladder, is essential for the digestion and absorption of dietary fats. It helps emulsify fats, breaking them down into smaller particles that can be easily digested by enzymes. This process promotes the absorption of vital fat-soluble vitamins and essential fatty acids.
Additionally, the gallbladder plays a crucial role in maintaining the balance of cholesterol in the body. Bile contains cholesterol, and when the gallbladder releases bile into the small intestine, it helps eliminate excess cholesterol from the body. This process prevents the buildup of cholesterol in the gallbladder, reducing the risk of gallstone formation.
Furthermore, the gallbladder acts as a storage unit for bile. It can hold up to 50 milliliters of bile, allowing for a constant supply to be released into the small intestine when needed. This storage capacity ensures a steady flow of bile to aid in the digestion of fats, even during periods of fasting or low-fat intake.
Why Gallbladder Removal is Necessary
Gallbladder removal, also known as cholecystectomy, becomes necessary when the gallbladder is affected by conditions such as gallstones or inflammation. These issues can lead to severe abdominal pain, indigestion, and other digestive complications. In some cases, like mine, the presence of gallstones disrupted the normal functioning of my gallbladder, exacerbating my IBS symptoms.
During a cholecystectomy, the gallbladder is surgically removed to alleviate the symptoms and prevent further complications. While the gallbladder is not an essential organ, its removal can have some effects on digestion. Without a gallbladder, bile is continuously released from the liver into the small intestine, rather than being stored and concentrated in the gallbladder. This can result in a more constant, but less concentrated, flow of bile, which may impact the digestion of fatty foods.
However, the human body is remarkably adaptable, and most individuals can adjust to the absence of a gallbladder. The liver compensates for the gallbladder's absence by producing smaller amounts of bile more frequently. This adaptation ensures that the necessary bile is still available for the digestion of fats, albeit in a slightly different manner.
It is important to note that while gallbladder removal may cause some changes in digestion, it is often a necessary procedure to alleviate pain and prevent complications. With advancements in medical technology, individuals who have undergone cholecystectomy can lead normal, healthy lives by making slight adjustments to their diet and lifestyle.
The Connection Between the Gallbladder and IBS
Research suggests a link between gallbladder dysfunction and IBS symptoms. The abnormal regulation of bile flow can impact the gut's motility and cause changes in bowel habits, leading to IBS-like symptoms. When the gallbladder is removed, the interruption in bile storage and release can trigger digestive issues, especially in individuals already susceptible to IBS.
How Gallbladder Removal Can Impact IBS
Following the removal of my gallbladder, my IBS symptoms underwent significant changes. While the pain associated with gallstones subsided, I experienced an increase in bloating, diarrhea, and overall gut discomfort. It took time to adjust to this new reality and discover effective coping strategies.
The Role of Bile in IBS Symptoms
Bile acid malabsorption, a condition that can occur after gallbladder removal, can contribute to the development or worsening of IBS symptoms. Bile acids, normally reabsorbed in the small intestine, may reach the large intestine in excess, causing irritation and diarrhea. It is essential to understand these dynamics to effectively manage IBS symptoms after gallbladder removal.
When the gallbladder is functioning properly, it stores bile produced by the liver and releases it into the small intestine to aid in the digestion of fats. Bile is a yellowish-green fluid that contains bile salts, cholesterol, bilirubin, and other substances. It helps break down fats into smaller molecules that can be easily absorbed by the body.
However, when the gallbladder is not functioning correctly, bile flow can be disrupted. This can lead to a buildup of bile in the gallbladder or a reflux of bile into the stomach or esophagus. The abnormal regulation of bile flow can affect the gut's motility, causing changes in bowel habits and contributing to the development of IBS symptoms.
After gallbladder removal, also known as cholecystectomy, the interruption in bile storage and release can have a significant impact on digestion. Without a gallbladder, bile is continuously released into the small intestine, which can overwhelm the digestive system and lead to digestive issues such as bloating, diarrhea, and gut discomfort.
Bile acid malabsorption is another factor that can contribute to the development or worsening of IBS symptoms after gallbladder removal. Bile acids, which are normally reabsorbed in the small intestine, may reach the large intestine in excess when bile flow is disrupted. This can cause irritation of the intestinal lining and lead to diarrhea.
Managing IBS symptoms after gallbladder removal can be challenging, but there are strategies that can help. It is important to work closely with a healthcare professional to develop an individualized treatment plan. This may include dietary modifications, such as avoiding trigger foods, increasing fiber intake, and consuming smaller, more frequent meals. Medications, such as bile acid binders or anti-diarrheal medications, may also be prescribed to help manage symptoms.
Additionally, stress management techniques, such as relaxation exercises or therapy, can be beneficial in reducing the impact of stress on IBS symptoms. Regular exercise and adequate sleep are also important for overall gut health.
In conclusion, the connection between the gallbladder and IBS is complex. Gallbladder dysfunction and its removal can have a significant impact on the development and management of IBS symptoms. Understanding the role of bile in digestion and the potential complications that can arise after gallbladder removal is crucial in effectively managing IBS symptoms and improving quality of life.
My Personal Journey with Gallbladder Removal and IBS
Pre-Surgery: My IBS Symptoms
Before the surgery, my IBS symptoms were already challenging to manage. I experienced frequent abdominal pain, alternating bowel habits, and unpredictable flare-ups. These symptoms made it difficult for me to lead a normal and comfortable life. I often found myself canceling plans or missing out on important events due to the debilitating pain and discomfort.
Living with IBS meant constantly being on edge, never knowing when the next flare-up would strike. It affected not only my physical well-being but also took a toll on my mental health. The constant worry and anxiety about having an IBS episode made it hard to fully enjoy life and engage in activities that I loved.
Despite trying various medications and following dietary recommendations, I struggled to find long-term relief. The presence of gallstones further complicated my condition, leading to the decision to remove my gallbladder. The hope was that by eliminating the gallbladder, my IBS symptoms would also improve.
Post-Surgery: Changes in My IBS Symptoms
After the surgery, my IBS symptoms underwent a noticeable transition. Initially, there was an overall improvement in the severity of my abdominal pain. The constant, sharp pain that used to plague me seemed to have subsided, bringing a sense of relief and optimism.
However, as I started to reintroduce solid foods into my diet, I noticed that my gut was more sensitive than ever. Certain foods that I used to enjoy without any issues now triggered bloating, gas, and diarrhea. It was frustrating to realize that the surgery, while beneficial in some aspects, had also introduced new challenges.
Understanding the connection between my gallbladder removal and the changes in my IBS symptoms required some research and consultation with my healthcare provider. It turns out that the gallbladder plays a role in the digestion and absorption of fats. Without it, the body may struggle to process certain foods, leading to digestive issues.
As I navigated this new phase of my journey, I had to make dietary and lifestyle adjustments to keep my symptoms in check. I started keeping a food diary to identify trigger foods and gradually eliminated them from my diet. It was a trial-and-error process, but over time, I discovered a list of foods that were more easily tolerated by my sensitive gut.
Additionally, I incorporated stress-management techniques into my daily routine. I found that stress had a significant impact on my IBS symptoms, and by practicing relaxation exercises, such as deep breathing and meditation, I was able to reduce the frequency and intensity of flare-ups.
While the road to managing my IBS symptoms post-gallbladder removal has been challenging, I have learned valuable lessons about self-care and resilience. I have become more attuned to my body's needs and have developed a greater appreciation for the importance of a balanced and mindful lifestyle.
Every day is a learning experience, and I continue to explore new strategies and treatments to further improve my quality of life. I am determined not to let IBS define me and am committed to finding ways to thrive despite the challenges it presents.
Coping Strategies for IBS After Gallbladder Removal
Dietary Adjustments for IBS Management
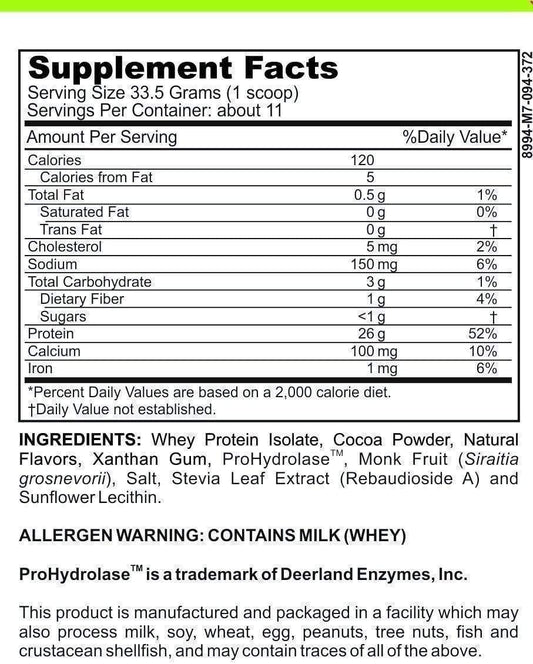
One of the most effective ways to manage IBS symptoms after gallbladder removal is through dietary adjustments. It is essential to identify trigger foods and make modifications accordingly. While each person's tolerance may differ, common triggers include fatty foods, spicy foods, caffeine, alcohol, and certain types of dairy. Opting for a low-fat, fiber-rich diet that includes lean proteins, fruits, and vegetables can help maintain a healthy digestive balance.
Lifestyle Changes to Ease IBS Symptoms
Aside from dietary modifications, certain lifestyle changes can greatly alleviate IBS symptoms. Stress management techniques such as mindfulness, meditation, and regular exercise have proven beneficial for many individuals. Engaging in regular physical activity not only promotes healthy bowel movements but also helps reduce stress levels, which can trigger IBS flare-ups.
Medical Treatments and Interventions for IBS Post-Gallbladder Removal
Medications to Control IBS Symptoms
In some cases, medical interventions may be necessary to manage more severe IBS symptoms post-gallbladder removal. Common medications prescribed include antispasmodics to alleviate abdominal pain and cramping, as well as certain medications that target diarrhea or constipation. It is crucial to consult with a healthcare provider to determine the most appropriate medication and dosage for individual needs.
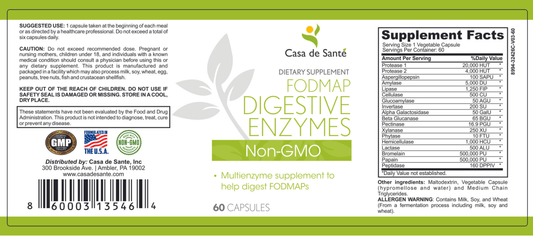
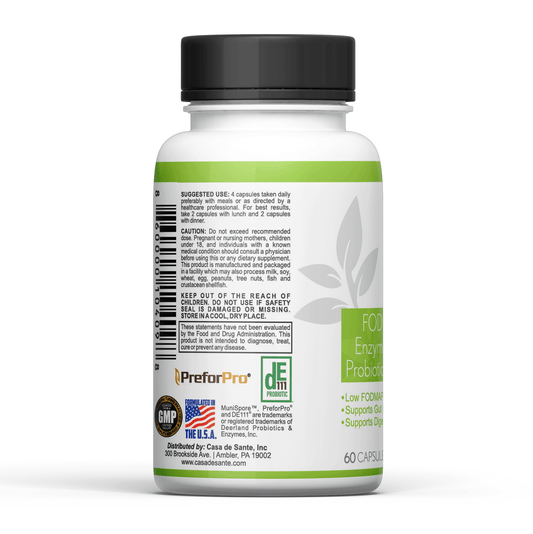
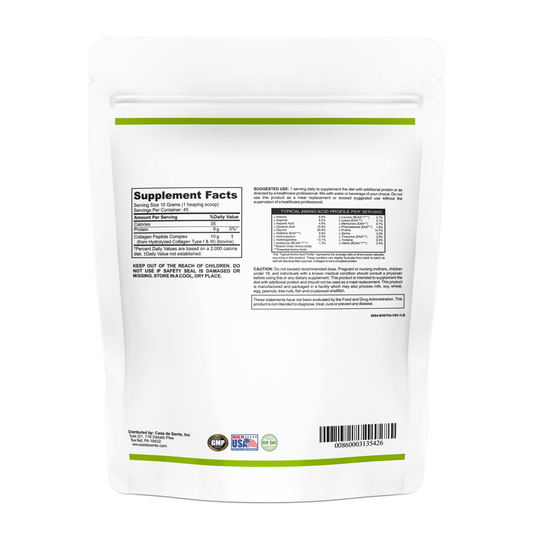
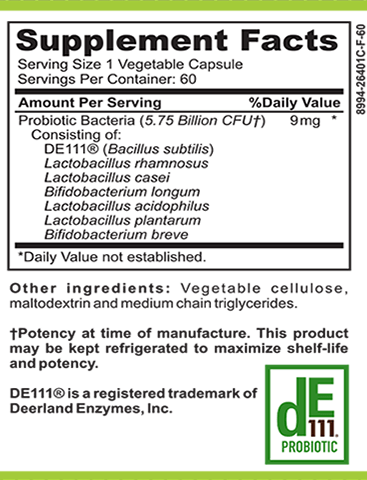
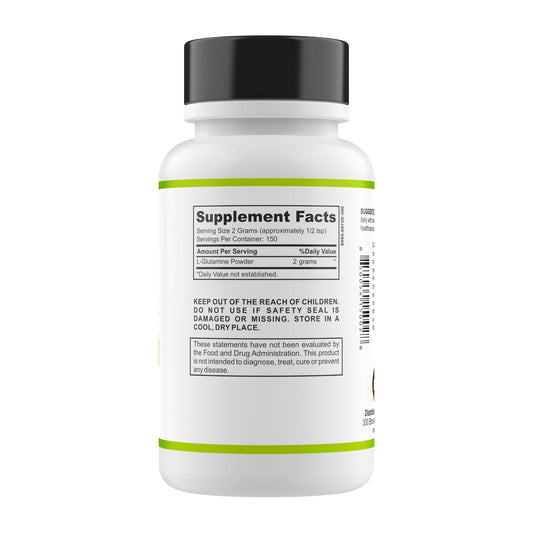
The Role of Probiotics and Digestive Enzymes
Supplementing with probiotics and digestive enzymes can also provide relief for those with IBS after gallbladder removal. Probiotics help restore the balance of healthy bacteria in the gut, promoting optimal digestion and reducing symptoms. Digestive enzymes aid in the breakdown of fats, assisting with the digestion of meals that may be challenging for individuals without a gallbladder.
In conclusion, having my gallbladder removed significantly impacted my IBS journey. Understanding the function of the gallbladder and its connection to IBS symptoms allowed me to take control of my health and develop effective coping strategies. Through dietary adjustments, lifestyle changes, and medical interventions when necessary, I have been able to manage my IBS and lead a fulfilling life post-gallbladder removal.