Does Stress Make IBS Worse?
Stress is a common part of daily life, and for individuals with irritable bowel syndrome (IBS), it can significantly impact their symptoms and overall quality of life. Understanding the connection between stress and IBS is crucial in managing this condition effectively. In this article, we dive into the science behind this connection, explore coping mechanisms for stress-induced IBS, discuss medical treatments, and take a look at the future of stress and IBS research.
Understanding the Connection Between Stress and IBS
Stress, defined as the body's response to mental or emotional pressure, can have a profound impact on bodily functions, including the digestive system. For individuals with IBS, stress often leads to symptom exacerbation and increased discomfort. It is important to recognize that stress is not the direct cause of IBS, but rather a trigger that can worsen existing symptoms.
Defining Stress and Its Impact on the Body
When we experience stress, our bodies release stress hormones such as cortisol and adrenaline. These hormones can disrupt the normal functioning of the digestive system, leading to an imbalance in gut bacteria and increased gut sensitivity. This, in turn, can result in symptoms such as abdominal pain, bloating, changes in bowel habits, and feelings of urgency.
Furthermore, stress can also affect the immune system, making individuals more susceptible to infections and inflammation in the gastrointestinal tract. This can further contribute to the development or exacerbation of IBS symptoms. The intricate relationship between stress and the body's physiological response highlights the importance of managing stress levels for individuals with IBS.
What is IBS: Symptoms and Triggers
Before delving deeper into the stress-IBS connection, it is crucial to understand what IBS is and what triggers its symptoms. IBS is a chronic disorder affecting the large intestine, characterized by recurring abdominal pain, bloating, and changes in bowel habits. Common triggers for IBS symptoms include certain foods, hormonal fluctuations, and, yes, stress.
Individuals with IBS may find that stressful situations, such as work deadlines, relationship issues, or major life events, can lead to an increase in their symptoms. This is because stress can disrupt the normal functioning of the gastrointestinal tract, leading to motility disturbances and heightened sensitivity to pain. The brain-gut connection plays a significant role in the manifestation of IBS symptoms, with stress acting as a powerful trigger.
Moreover, the relationship between stress and IBS is bidirectional. While stress can worsen IBS symptoms, the presence of chronic symptoms can also contribute to increased stress levels. The constant worry and anxiety associated with unpredictable bowel movements and abdominal discomfort can create a vicious cycle, further exacerbating the condition.
It is important to note that not all individuals with IBS experience stress as a trigger for their symptoms. Each person's experience with IBS is unique, and while stress plays a significant role for some, it may not be the primary trigger for others. Understanding the individual factors that contribute to symptom exacerbation is crucial in developing personalized management strategies.
In conclusion, the connection between stress and IBS is complex and multifaceted. Stress can disrupt the normal functioning of the digestive system, leading to an increase in IBS symptoms. Conversely, the presence of chronic symptoms can also contribute to heightened stress levels. Managing stress through various techniques such as relaxation exercises, therapy, and lifestyle modifications can be beneficial in reducing symptom severity and improving overall quality of life for individuals with IBS.
The Science Behind Stress and IBS
While the exact mechanisms behind the stress-IBS connection are not yet fully understood, research has shed light on several key factors:
The Role of the Gut-Brain Axis
The gut-brain axis refers to the bidirectional communication system between the gut and the brain. It is a complex network of nerves, hormones, and biochemical signals that allows for constant communication and coordination between these two vital systems. Stress can disrupt this communication, leading to alterations in gut motility, increased gut permeability, and heightened inflammation, all of which contribute to worsened IBS symptoms.
When we experience stress, the brain releases various neurotransmitters and hormones that can directly affect the gut. For example, the release of stress hormones like cortisol and adrenaline can stimulate the release of substances that promote inflammation in the gut. This inflammation can disrupt the normal functioning of the intestines, leading to symptoms such as abdominal pain, bloating, and changes in bowel habits.
Furthermore, stress can also affect the balance of the gut microbiota, which refers to the trillions of microorganisms that inhabit our digestive tract. These microorganisms play a crucial role in maintaining gut health and proper digestion. Stress-induced alterations in the gut microbiota composition and diversity have been observed in individuals with IBS, suggesting a potential link between stress, gut bacteria, and IBS symptoms.
Hormonal Responses to Stress and Their Effects on IBS
Stress triggers the release of stress hormones, such as cortisol and adrenaline, which can impact the digestive system in multiple ways. These hormones are part of the body's natural response to stress, preparing us for a "fight or flight" response. However, in the context of chronic stress, the prolonged elevation of stress hormones can have detrimental effects on the gut and worsen IBS symptoms.
High levels of cortisol, for example, can increase intestinal permeability, also known as "leaky gut." This means that the lining of the intestines becomes more porous, allowing substances that would normally be restricted to pass through and enter the bloodstream. This can trigger an immune response and further contribute to inflammation in the gut, exacerbating IBS symptoms.
In addition, stress hormones can also affect the production of mucus in the gut. Mucus acts as a protective barrier, preventing harmful substances from coming into direct contact with the delicate lining of the intestines. However, under chronic stress, cortisol can reduce the production of this protective mucus, leaving the gut more vulnerable to irritation and damage.
Furthermore, stress can influence the release of other hormones involved in digestion, such as gastrin and motilin, which regulate stomach acid secretion and gut motility, respectively. Imbalances in these hormones can disrupt the normal digestive process and contribute to IBS symptoms, including abdominal pain, diarrhea, and constipation.
Overall, while the exact mechanisms linking stress and IBS are still being unraveled, the gut-brain axis and hormonal responses to stress play significant roles in the development and exacerbation of IBS symptoms. Understanding these intricate connections can help guide future research and potentially lead to more effective treatments for individuals with stress-related IBS.
Coping Mechanisms for Stress-Induced IBS
Living with stress-induced irritable bowel syndrome (IBS) can be challenging, as stress can exacerbate symptoms and make everyday life more difficult. While complete elimination of stress is unlikely, there are several coping mechanisms that can help individuals manage stress-induced IBS effectively and improve their quality of life.
Stress Management Techniques for IBS Patients
Engaging in stress-reduction activities can be highly beneficial for individuals with stress-induced IBS. Practices such as meditation, deep breathing exercises, yoga, and mindfulness have been shown to reduce stress levels and restore balance to the gut-brain axis. These techniques help individuals relax, focus their minds, and alleviate the physical and emotional toll that stress can have on the body.
In addition to these practices, regular exercise and getting enough sleep also play a crucial role in managing stress and improving overall well-being. Exercise releases endorphins, which are natural mood boosters, and helps reduce stress hormones in the body. Getting enough sleep is equally important, as sleep deprivation can increase stress levels and worsen IBS symptoms. Establishing a consistent sleep routine and creating a calming sleep environment can greatly contribute to stress reduction.
Dietary Adjustments to Alleviate IBS Symptoms
Adopting dietary changes can also be beneficial in managing stress-induced IBS. Avoiding trigger foods is key to minimizing symptoms. Spicy foods, caffeine, alcohol, and fatty foods are known to aggravate IBS symptoms and should be avoided or consumed in moderation. By identifying and eliminating trigger foods, individuals can significantly reduce the frequency and severity of their symptoms.
Incorporating a high-fiber diet can also help alleviate IBS symptoms. Fiber adds bulk to the stool, promoting regular bowel movements and reducing discomfort. Foods rich in fiber include fruits, vegetables, whole grains, and legumes. It is important to gradually increase fiber intake to avoid sudden changes in bowel habits, which can trigger symptoms. Staying well-hydrated is equally important, as it helps soften the stool and prevent constipation.
Furthermore, keeping a food diary can be helpful in identifying specific foods that trigger IBS symptoms. By tracking what they eat and how it affects their symptoms, individuals can make informed decisions about their diet and identify patterns that can guide them in managing their condition effectively.
In conclusion, while stress-induced IBS can be challenging to manage, there are coping mechanisms that can significantly improve symptoms and overall well-being. Engaging in stress reduction techniques, such as meditation and exercise, and making dietary adjustments, such as avoiding trigger foods and incorporating a high-fiber diet, can help individuals regain control over their lives and minimize the impact of stress on their IBS symptoms.
Medical Treatments for Stress-Related IBS
For individuals with severe or persistent symptoms, medical treatments may be necessary to alleviate stress-related IBS:
Medications to Control IBS Symptoms
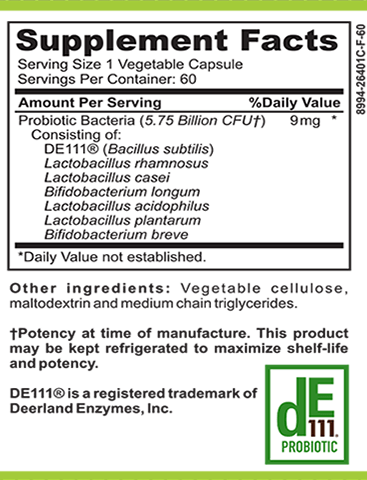
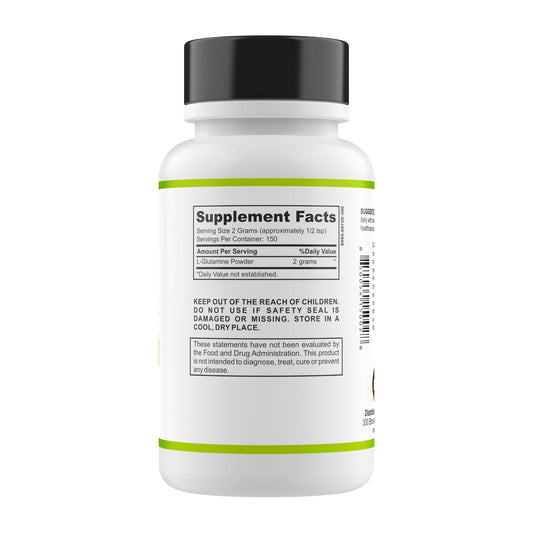
Antispasmodic medications can help relieve abdominal pain and cramping. Probiotics, on the other hand, can restore gut microbial balance and reduce inflammation. In some cases, doctors may prescribe low-dose antidepressants, which can modulate pain sensations in the gut and improve overall symptoms.
Psychological Therapies for Stress Management
Psychological therapies, such as cognitive-behavioral therapy (CBT) and gut-directed hypnotherapy, can help individuals develop effective coping strategies for managing stress-induced IBS. These therapies focus on identifying and modifying negative thought patterns and behaviors, reducing stress levels, and improving overall quality of life.
The Future of Stress and IBS Research
While significant progress has been made in understanding the stress-IBS connection, there is still much to learn. Ongoing research aims to uncover potential breakthroughs in IBS treatment:
Potential Breakthroughs in IBS Treatment
Scientists are exploring innovative therapies such as fecal microbiota transplantation (FMT) and neuromodulation techniques to treat IBS. These cutting-edge approaches could provide new avenues for managing stress-related symptoms and improving the overall well-being of individuals living with IBS.
The Importance of Continued Research into Stress and IBS
Continued research into the stress-IBS connection is vital in improving our understanding of this complex relationship. By deepening our knowledge of the mechanisms involved, researchers can develop more targeted treatments that address the underlying causes of stress-induced IBS, ultimately providing relief for those affected.
In conclusion, stress can undeniably make IBS symptoms worse for individuals living with this chronic condition. By recognizing the connection between stress and IBS, implementing coping mechanisms, considering medical treatments, and supporting ongoing research, individuals with IBS have the opportunity to better manage their symptoms and improve their overall well-being.