Vitamin B12 in Crohn's Disease and Ulcerative Colitis: The Essential Guide
Vitamin B12 is a crucial nutrient needed for maintaining optimal health, especially for individuals with inflammatory bowel diseases (IBD) such as Crohn's disease and ulcerative colitis. In this comprehensive guide, we will explore the role of vitamin B12 in Crohn's disease and ulcerative colitis, common causes of deficiency, symptoms, and how to manage these conditions effectively.
Table of Contents
- The Importance of Vitamin B12
- Vitamin B12 and Inflammatory Bowel Disease
- Causes of Vitamin B12 Deficiency in Crohn's Disease and Ulcerative Colitis
- Symptoms of Vitamin B12 Deficiency
- Diagnosis of Vitamin B12 Deficiency in IBD
- Treatment and Management of Vitamin B12 Deficiency
- Dietary Sources of Vitamin B12
- Supplementation and Absorption
- The Role of Genetics in Vitamin B12 Absorption
- Casa de Sante: Your Partner in Gut Health
1. The Importance of Vitamin B12
Vitamin B12, also known as cobalamin, is an essential nutrient that plays a vital role in various biological processes. Some of its primary functions include:
- Formation of red blood cells
- Transmission of nerve signals
- Production of DNA
- Energy generation
As our bodies cannot synthesize vitamin B12, we must obtain it through our diet or supplements. Adequate intake of this nutrient is crucial for overall health and well-being.
2. Vitamin B12 and Inflammatory Bowel Disease
Inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, are chronic conditions characterized by inflammation in the digestive system. These disorders can lead to malabsorption of nutrients, including vitamin B12. Therefore, individuals with IBD may be at a higher risk of developing vitamin B12 deficiency.
3. Causes of Vitamin B12 Deficiency in Crohn's Disease and Ulcerative Colitis
There are several factors that can contribute to vitamin B12 deficiency in individuals with Crohn's disease and ulcerative colitis, including:
3.1 Reduced Absorption
Vitamin B12 absorption primarily occurs in the terminal ileum of the small intestine. Inflammation or surgical removal of this part of the intestine, as seen in Crohn's disease and some cases of ulcerative colitis, can result in impaired absorption of vitamin B12.
3.2 Medication Use
Certain medications, such as proton pump inhibitors (PPIs) that are prescribed to IBD patients for managing stomach ulcers or acid reflux, can interfere with vitamin B12 absorption. PPIs reduce stomach acid production, which is necessary for the absorption of B12 in the small intestine.
3.3 Dietary Limitations
Individuals with IBD may follow restrictive diets, eliminating or limiting their intake of foods rich in vitamin B12. This can result in inadequate levels of the nutrient in the body.
4. Symptoms of Vitamin B12 Deficiency
The symptoms of vitamin B12 deficiency can vary but often include:
- Fatigue
- Weakness
- Pale skin
- Shortness of breath
- Heart palpitations
- Nerve problems (e.g., numbness or tingling in hands and feet)
- Vision loss
- Mental health issues (e.g., depression, memory problems)
If you suspect vitamin B12 deficiency, consult your healthcare provider for proper evaluation and treatment.
5. Diagnosis of Vitamin B12 Deficiency in IBD
Diagnosing vitamin B12 deficiency in individuals with IBD can be challenging due to the overlapping symptoms with the underlying bowel disease. However, a combination of serum vitamin B12 levels and methylmalonic acid (MMA) concentrations can help determine the true deficiency. Healthcare providers may also consider other factors, such as patient's medical history, disease severity, and genetic predisposition, to make an accurate diagnosis.
6. Treatment and Management of Vitamin B12 Deficiency
The management of vitamin B12 deficiency in IBD patients typically involves:
6.1 Supplementation
Oral or injectable vitamin B12 supplements may be prescribed to increase the levels of the nutrient in the body.
6.2 Dietary Modifications
Incorporating vitamin B12-rich foods into the diet can help improve nutrient levels. Additionally, working with a registered dietitian can ensure a balanced diet that meets the individual's nutritional needs.
6.3 Monitoring
Regular monitoring of vitamin B12 levels is essential to ensure appropriate treatment and prevent recurrence of deficiency.
7. Dietary Sources of Vitamin B12
Vitamin B12 is primarily found in animal-based products and fortified foods. Some common sources include:
- Meat
- Poultry
- Eggs
- Dairy products
- Some cheeses
- Fortified cereals
- Fortified non-dairy milk
- Nutritional yeast
It is important for individuals with IBD to consume a balanced diet that includes adequate amounts of vitamin B12.
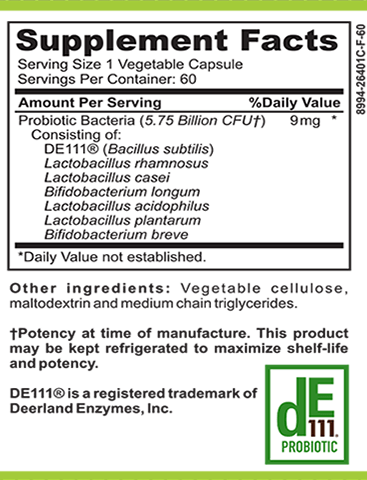
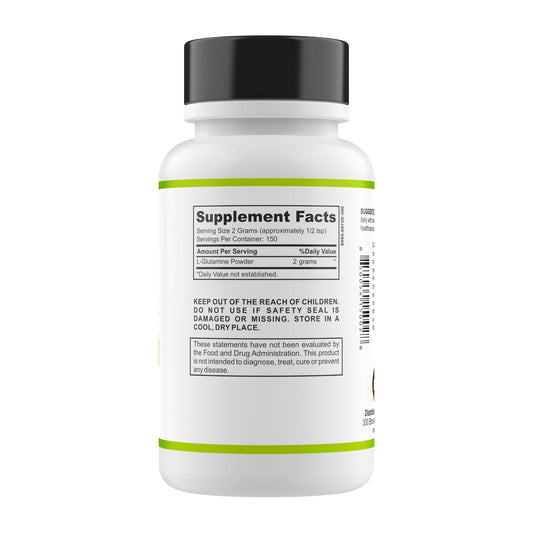
8. Supplementation and Absorption
Oral supplementation is often the first line of treatment for vitamin B12 deficiency. However, in cases of severe malabsorption, healthcare providers may recommend intramuscular injections to ensure adequate levels of the nutrient.
It is essential to discuss supplementation options with your healthcare provider to determine the most suitable form and dosage for your specific needs.
9. The Role of Genetics in Vitamin B12 Absorption
Genetic factors may influence an individual's ability to absorb vitamin B12. For example, mutations in the fucosyltransferase 2 (FUT2) gene have been associated with altered vitamin B12 status. Understanding one's genetic predisposition can aid in the appropriate management of vitamin B12 deficiency in IBD patients.
10. Casa de Sante: Your Partner in Gut Health
Casa de Sante is a leading virtual dietitian support platform for individuals with IBD, food sensitivities, and other digestive disorders. Our expert team of registered dietitians and health coaches can help you manage your condition through personalized care, comprehensive testing, and valuable educational resources.
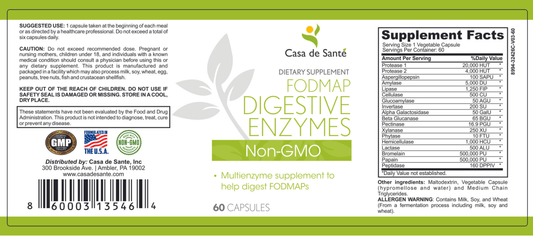
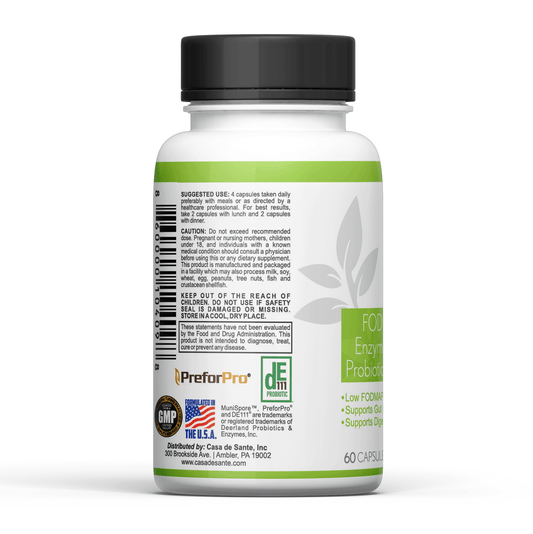
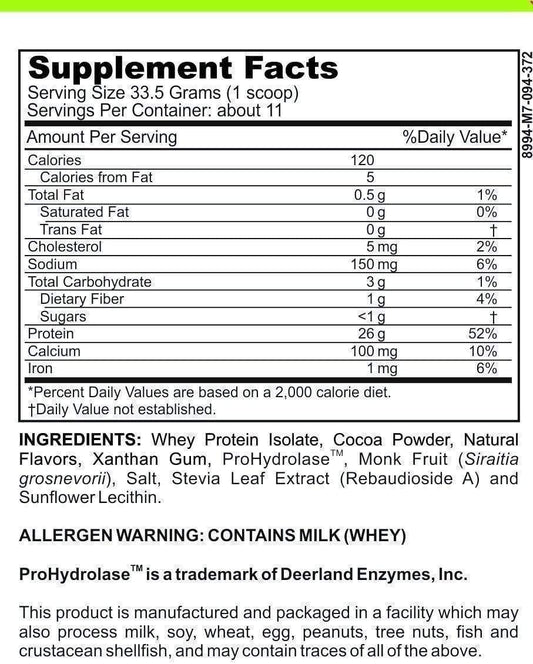
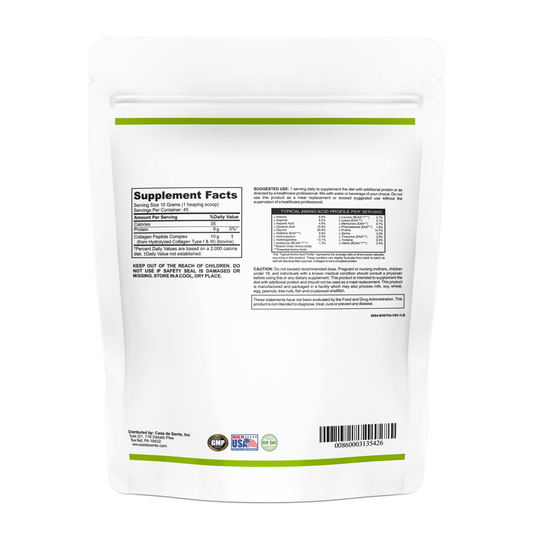
Discover our specially formulated low FODMAP products, including seasonings, protein powders, and supplements, designed for sensitive digestive systems. Keep track of your symptoms and follow your personalized diet using our gut health apps.
Take the first step towards relief with a free gut health assessment. Visit our website now and start your journey to better gut health.