Pediatric IBD: Inflammatory Bowel Disease Explained
Inflammatory Bowel Disease (IBD) is a term that describes conditions characterized by chronic inflammation of the gastrointestinal (GI) tract. The two most common types are Crohn's disease and ulcerative colitis. While IBD can affect anyone, this article focuses on pediatric IBD, which refers to these conditions when they occur in children and adolescents.
Understanding pediatric IBD is crucial because it presents unique challenges compared to adult-onset IBD. The disease can significantly impact a child's growth, development, and quality of life. This article aims to provide a comprehensive understanding of pediatric IBD, its types, symptoms, causes, diagnosis, treatment, and management.
Types of Pediatric IBD
There are two main types of IBD that can occur in children: Crohn's disease and ulcerative colitis. Both conditions involve chronic inflammation of the GI tract, but they differ in the areas affected and the depth of inflammation.
Crohn's disease can affect any part of the GI tract from the mouth to the anus, and inflammation can occur in all layers of the bowel walls. Ulcerative colitis, on the other hand, is limited to the colon (large intestine) and the rectum, and inflammation is usually confined to the innermost lining of the colon.
Crohn's Disease in Children
Crohn's disease can occur at any age, but it is often diagnosed in adolescents and young adults. In children, it can cause significant complications, including growth delay, malnutrition, and bone health issues. The symptoms can vary widely and may include abdominal pain, diarrhea, bloody stools, weight loss, and fatigue.
Children with Crohn's disease may also experience symptoms outside the GI tract, such as joint pain, skin problems, and eye inflammation. The disease course can vary greatly from child to child, with some experiencing mild symptoms and others having severe, debilitating disease.
Ulcerative Colitis in Children
Ulcerative colitis typically begins in the rectum and may extend upward into the colon. The disease is often diagnosed in late adolescence, but it can occur at any age. Children with ulcerative colitis may experience symptoms such as bloody diarrhea, abdominal pain, weight loss, and fatigue.
Like Crohn's disease, ulcerative colitis can also affect growth and development in children. Additionally, it can cause extraintestinal symptoms such as joint pain, skin problems, and eye inflammation. The severity and course of the disease can vary widely among children.
Causes and Risk Factors of Pediatric IBD
The exact cause of pediatric IBD is unknown, but it is thought to result from a combination of genetic, environmental, and immune system factors. Some children may have a genetic predisposition to IBD, which, when triggered by certain environmental factors, leads to an abnormal immune response and chronic inflammation in the GI tract.
Several risk factors have been identified for pediatric IBD. These include having a family history of IBD, certain genetic mutations, exposure to secondhand smoke, and certain dietary factors. However, many children with IBD do not have any of these risk factors, indicating that the causes of the disease are complex and not fully understood.
Genetic Factors
Research has identified several genes that are associated with an increased risk of IBD. These genes are involved in various functions, including immune response, bacterial defense, and maintenance of the intestinal barrier. Children who have a parent or sibling with IBD are at a higher risk of developing the disease.
However, not everyone who inherits these genetic mutations will develop IBD, suggesting that other factors, such as environmental triggers or an abnormal immune response, are also involved in the disease's development.
Environmental Factors
Environmental factors are thought to play a role in triggering IBD in genetically susceptible individuals. These factors can include infections, antibiotic use, diet, and exposure to secondhand smoke. However, the exact role of these factors in the development of pediatric IBD is still under investigation.
For example, some studies suggest that a diet high in processed foods and low in fruits and vegetables may increase the risk of IBD. Additionally, exposure to secondhand smoke during childhood has been associated with an increased risk of Crohn's disease. However, more research is needed to confirm these findings and understand how these factors contribute to the disease.
Diagnosis of Pediatric IBD
Diagnosing pediatric IBD can be challenging due to the wide range of symptoms and the overlap with other conditions. The diagnosis is usually based on a combination of clinical symptoms, laboratory tests, imaging studies, and endoscopic evaluation with biopsy.
The first step in diagnosing IBD is a thorough medical history and physical examination. The doctor will ask about the child's symptoms, family history of IBD, and any medications or dietary supplements the child is taking. The physical examination may include checking for abdominal pain, growth delay, and signs of malnutrition.
Laboratory Tests
Laboratory tests can help support the diagnosis of IBD and assess the disease's severity. These tests may include blood tests to check for anemia, inflammation, and malnutrition, and stool tests to look for infection or bleeding in the GI tract.
However, these tests cannot confirm the diagnosis of IBD, as they can be abnormal in many other conditions. Therefore, if the results suggest IBD, further testing is usually needed to confirm the diagnosis.
Endoscopic Evaluation with Biopsy
Endoscopy is a procedure that allows the doctor to look directly at the inside of the GI tract. In children suspected of having IBD, a colonoscopy and often an upper endoscopy are performed. During these procedures, small samples of tissue (biopsies) are taken for examination under a microscope.
The endoscopic findings and biopsy results can help confirm the diagnosis of IBD and differentiate between Crohn's disease and ulcerative colitis. They can also help assess the severity of the disease and guide treatment decisions.
Treatment of Pediatric IBD
The goal of treatment in pediatric IBD is to induce and maintain remission, improve quality of life, and promote normal growth and development. The treatment plan is individualized based on the child's age, disease type, severity, and response to previous treatments.
Treatment options for pediatric IBD include medications, dietary therapy, and in some cases, surgery. It's important to note that while these treatments can manage the symptoms and complications of IBD, they cannot cure the disease.
Medications
Medications are the mainstay of treatment for pediatric IBD. They work by reducing inflammation in the GI tract, relieving symptoms, and preventing flare-ups. The choice of medication depends on the type and severity of the disease, as well as the child's response to previous treatments.
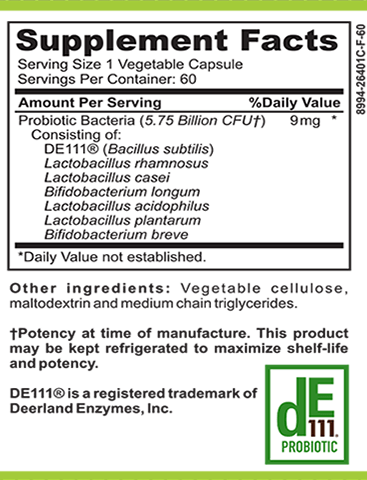
Commonly used medications for pediatric IBD include aminosalicylates, corticosteroids, immunomodulators, and biologic therapies. Each of these medications has its benefits and risks, and the decision to use a particular medication should be made in consultation with the child's healthcare provider.
Dietary Therapy
Dietary therapy can play a role in managing pediatric IBD. Certain diets may help reduce inflammation and symptoms, and in some cases, may be used as a primary treatment. However, dietary therapy should not replace medical therapy unless recommended by the child's healthcare provider.
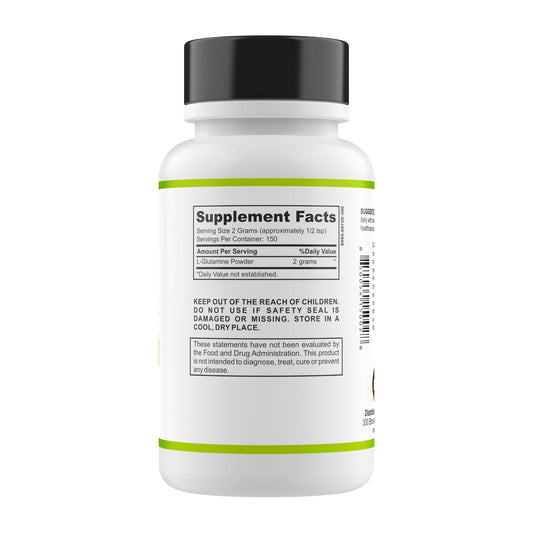
One commonly used dietary therapy is the exclusive enteral nutrition (EEN), which involves replacing all regular food with a special liquid formula for a certain period. This therapy has been shown to be effective in inducing remission in children with Crohn's disease. Other dietary approaches, such as the specific carbohydrate diet (SCD) and the Mediterranean diet, are also being studied for their potential benefits in IBD.
Surgery
Surgery may be needed in some children with IBD, particularly those with severe disease that does not respond to medical therapy. The type of surgery depends on the type and location of the disease, as well as the child's overall health.
For children with Crohn's disease, surgery may involve removing a section of the diseased bowel. For those with ulcerative colitis, surgery may involve removing the entire colon and rectum. While surgery can provide significant relief from symptoms, it is not a cure and the disease can recur.
Management of Pediatric IBD
Managing pediatric IBD involves more than just treating the disease. It also involves addressing the physical, emotional, and social challenges that come with living with a chronic illness. This often requires a multidisciplinary approach, involving a team of healthcare providers including a pediatric gastroenterologist, dietitian, psychologist, and social worker.
Management strategies may include regular monitoring of growth and development, nutritional support, psychological support, and school support. It's also important for children with IBD and their families to have access to accurate information about the disease and to be involved in decision-making about their care.
Nutritional Support
Nutritional support is a key component of managing pediatric IBD. Children with IBD are at risk of malnutrition due to decreased food intake, malabsorption, and increased nutrient needs. A dietitian can provide individualized dietary advice to ensure the child is getting the necessary nutrients for growth and development.
In some cases, supplemental nutrition may be needed. This can be provided orally, or in more severe cases, through a feeding tube. The goal of nutritional support is not only to improve nutritional status but also to promote healing of the GI tract and reduce inflammation.
Psychological Support
Living with a chronic illness like IBD can be emotionally challenging for children and their families. Children with IBD may experience feelings of fear, anxiety, and depression, and may have difficulty coping with their disease. A psychologist or counselor can provide support and teach coping strategies to help manage these challenges.
Support groups can also be helpful, providing a safe space for children and their families to share their experiences and learn from others who are going through similar challenges. Online resources and educational materials can also provide valuable information and support.
School Support
IBD can affect a child's school performance and attendance due to frequent absences, fatigue, and difficulty concentrating. It's important for the school to be aware of the child's condition and to provide necessary accommodations. This may include allowing extra time for tests, providing a place to rest, and allowing access to the bathroom as needed.
Communication between the healthcare team, the school, and the family is crucial in ensuring the child's academic needs are met. A social worker can help facilitate this communication and advocate for the child's rights.
In conclusion, pediatric IBD is a complex condition that requires comprehensive care. With appropriate treatment and management, most children with IBD can lead healthy, fulfilling lives. Ongoing research continues to improve our understanding of this disease and develop more effective treatments.