Immune System: Inflammatory Bowel Disease Explained
The immune system plays a crucial role in the development and progression of Inflammatory Bowel Disease (IBD), a chronic condition characterized by inflammation of the digestive tract. Understanding the complex interplay between the immune system and IBD can provide valuable insights into the pathogenesis, diagnosis, and treatment of this debilitating disease.
Inflammatory Bowel Disease is a term that encompasses two primary conditions: Crohn's disease and Ulcerative Colitis. Both conditions involve chronic inflammation of the gastrointestinal tract, but they differ in the areas affected and the depth of inflammation. The immune system's role in these diseases is a subject of extensive research and is key to understanding their development and progression.
Understanding the Immune System
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful invaders, such as bacteria, viruses, and other foreign substances. It is designed to recognize and eliminate these threats to maintain the body's health and integrity.
However, in some cases, the immune system can mistakenly identify normal, healthy cells as foreign and launch an attack against them. This is known as an autoimmune response, and it is a key factor in the development of IBD. Understanding how this occurs is crucial to understanding the disease itself.
Components of the Immune System
The immune system is composed of various components, each playing a unique role in defending the body. These include white blood cells (leukocytes), which are further divided into two main types: lymphocytes (B cells and T cells) and phagocytes. B cells produce antibodies that neutralize foreign substances, while T cells destroy compromised cells. Phagocytes, on the other hand, engulf and destroy invaders.
Other components include the lymphatic system, which transports and filters lymph fluid containing white blood cells, and the spleen, which produces white blood cells and filters the blood. The immune system also includes the thymus, where T cells mature, and bone marrow, which produces red and white blood cells.
Immune Response
The immune response is a complex process that involves the activation of various immune cells and the release of signaling molecules, known as cytokines. When a foreign substance enters the body, immune cells recognize it as a threat and trigger an immune response. This involves the production of antibodies by B cells, the activation of T cells, and the release of cytokines to coordinate the response.
In a healthy immune response, the threat is neutralized, and the immune system returns to a state of rest. However, in autoimmune conditions like IBD, the immune system remains active, leading to chronic inflammation and tissue damage.
Immune System and Inflammatory Bowel Disease
In IBD, the immune system plays a central role. It is believed that a combination of genetic and environmental factors triggers an abnormal immune response in the gut, leading to chronic inflammation. This inflammation can cause a range of symptoms, including abdominal pain, diarrhea, weight loss, and fatigue.
Research has shown that people with IBD have an overactive immune system in their gut. This leads to the release of a large number of cytokines, causing inflammation and damage to the intestinal lining. Understanding the specific immune processes involved in IBD can help in the development of targeted therapies.
Role of T Cells in IBD
T cells, a type of white blood cell, play a crucial role in the immune response associated with IBD. In healthy individuals, T cells help protect the body from harmful invaders. However, in people with IBD, T cells in the gut can become overactive and cause inflammation.
Research has shown that certain types of T cells, known as Th1 and Th17 cells, are particularly active in people with IBD. These cells produce a large amount of pro-inflammatory cytokines, which contribute to the inflammation seen in IBD. Targeting these cells and their cytokines is a key area of research in IBD treatment.
Role of Gut Microbiota in IBD
The gut microbiota, the community of microorganisms living in our intestines, also plays a crucial role in IBD. In healthy individuals, the gut microbiota and the immune system exist in a state of balance, with the microbiota helping to regulate the immune response. However, in people with IBD, this balance is disrupted, leading to an overactive immune response and inflammation.
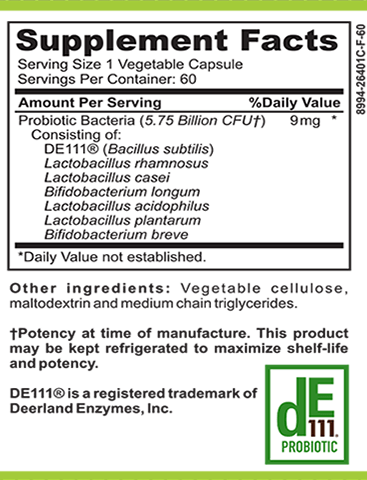
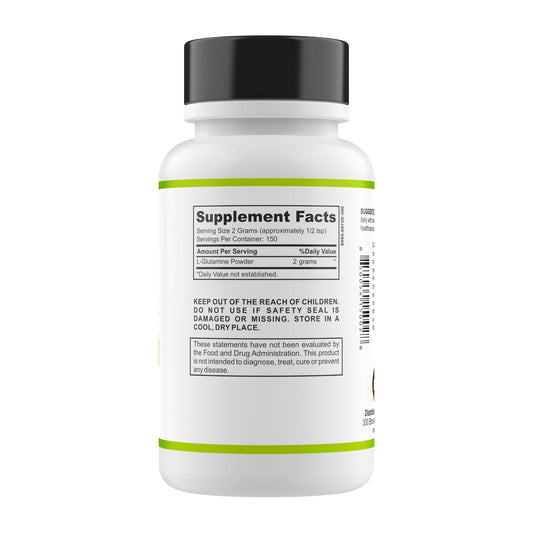
Research has shown that people with IBD have a different composition of gut microbiota compared to healthy individuals. This dysbiosis, or imbalance, may contribute to the overactive immune response seen in IBD. Restoring this balance through probiotics or fecal microbiota transplantation is a promising area of research in IBD treatment.
Diagnosis of Inflammatory Bowel Disease
Diagnosing IBD involves a combination of clinical evaluation, laboratory tests, imaging studies, and endoscopic procedures. The goal is to confirm the presence of chronic inflammation in the gut and to differentiate between Crohn's disease and ulcerative colitis, the two main types of IBD.
Immune markers, such as antibodies and cytokines, can also be used in the diagnosis of IBD. These markers can provide valuable information about the immune response and can help guide treatment decisions.
Endoscopy and Biopsy
Endoscopy is a key tool in the diagnosis of IBD. This procedure involves the use of a flexible tube with a camera to visualize the inside of the digestive tract. In people with IBD, endoscopy can reveal signs of inflammation, such as redness, swelling, and ulcers.
A biopsy, or tissue sample, can also be taken during endoscopy. This sample can be examined under a microscope to confirm the presence of inflammation and to look for changes in the cells that may indicate IBD.
Imaging Studies
Imaging studies, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), can also be used in the diagnosis of IBD. These tests can provide detailed images of the digestive tract and can reveal signs of inflammation and damage.
For example, a CT scan can show thickening of the intestinal wall, a common sign of IBD. An MRI can provide detailed images of the small intestine, an area that is difficult to reach with endoscopy.
Treatment of Inflammatory Bowel Disease
The treatment of IBD focuses on reducing inflammation, relieving symptoms, and preventing complications. This often involves a combination of medication, lifestyle changes, and in some cases, surgery.
Understanding the role of the immune system in IBD has led to the development of targeted therapies that can modulate the immune response. These include biologic drugs, such as anti-TNF agents, which block the action of a key inflammatory cytokine, and immunomodulators, which suppress the immune system to reduce inflammation.
Medication
Medication is a key component of IBD treatment. Anti-inflammatory drugs, such as aminosalicylates and corticosteroids, are often used to reduce inflammation and relieve symptoms. However, these drugs do not work for everyone, and they can have side effects, especially with long-term use.
Biologic drugs and immunomodulators offer a more targeted approach. These drugs work by blocking specific components of the immune response, reducing inflammation without the broad effects of corticosteroids. However, they can also have side effects, and their use must be carefully monitored.
Surgery
In some cases, when medication is not effective or complications arise, surgery may be necessary. This can involve removing a portion of the diseased intestine or creating a stoma, an opening in the abdomen to divert waste from the body.
While surgery can provide relief from symptoms, it is not a cure for IBD. The disease can recur in other parts of the digestive tract. Therefore, ongoing medical treatment is often necessary even after surgery.
Conclusion
The immune system plays a crucial role in the development and progression of Inflammatory Bowel Disease. Understanding this complex relationship can provide valuable insights into the pathogenesis, diagnosis, and treatment of this debilitating disease.
While much progress has been made in understanding the immune processes involved in IBD, there is still much to learn. Ongoing research in this area holds the promise of new and more effective treatments for this challenging condition.