Understanding Histamine Intolerance: Causes, Symptoms, and Management
Histamine intolerance is a condition that affects many individuals and can have wide-ranging symptoms. Understanding the causes, symptoms, and management options can be key to improving the quality of life for those affected by this intolerance. In this article, we will explore the role of histamine in the body, uncover the triggers of histamine release, discuss the impact of excess histamine on the body, and delve into the factors that contribute to high histamine levels. We will also discuss the symptoms of histamine intolerance, provide insights into the foods to avoid, explore treatment options, and touch on the feasibility of testing for histamine intolerance. Finally, we will discuss various strategies for managing and treating histamine intolerance.
Understanding Histamine Intolerance
Exploring the Role of Histamine in the Body
Histamine is a natural compound found in the body that is involved in various physiological processes. It functions as a neurotransmitter, helping to transmit signals in the brain, and also acts as a regulator of the immune response. Histamine plays a crucial role in the body's defense against foreign substances, but excessive levels can lead to adverse effects.
In individuals with histamine intolerance, the body is unable to break down histamine efficiently, resulting in an accumulation of this compound. This can trigger a wide range of symptoms that vary from person to person, making it essential to understand the underlying causes.
When histamine is released in the body, it binds to specific receptors, including H1, H2, H3, and H4 receptors, located in various tissues. Activation of these receptors leads to different physiological responses. For example, activation of H1 receptors can cause smooth muscle contraction, leading to symptoms such as nasal congestion and bronchoconstriction. On the other hand, activation of H2 receptors can stimulate gastric acid secretion, contributing to digestive issues.
Uncovering the Triggers of Histamine Release
Histamine release can be triggered by various factors, including certain foods, environmental allergens, stress, and medications. Understanding these triggers is crucial in managing histamine intolerance effectively.
Common dietary triggers include fermented foods, aged cheeses, alcohol, and processed meats. These foods contain high levels of histamine or can stimulate the release of histamine in the body. It is important for individuals with histamine intolerance to be aware of these triggers and make dietary adjustments accordingly.
Environmental allergens such as pollen, dust mites, and pet dander can also stimulate histamine release. When exposed to these allergens, the immune system reacts by releasing histamine, leading to allergic symptoms such as itching, sneezing, and watery eyes.
Additionally, stress and certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can contribute to elevated histamine levels. Stress can stimulate the release of histamine in the body, exacerbating symptoms of histamine intolerance. Certain medications, particularly NSAIDs, can inhibit the activity of enzymes responsible for breaking down histamine, leading to its accumulation.
The Impact of Excess Histamine on the Body
Excess histamine in the body can lead to a range of symptoms, including but not limited to headaches, nasal congestion, itching, hives, digestive issues, and fatigue. These symptoms can significantly affect an individual's daily life and overall well-being. Identifying the impact of excess histamine is crucial in managing the condition effectively.
Headaches are a common symptom of histamine intolerance and can range from mild to severe. They can be accompanied by other symptoms such as dizziness and sensitivity to light and sound. Nasal congestion, often referred to as a "stuffy nose," can make breathing difficult and affect sleep quality.
Itching and hives are another manifestation of histamine intolerance. Itchy skin can be localized or widespread and may be accompanied by redness and swelling. Digestive issues, such as abdominal pain, bloating, and diarrhea, can occur due to histamine's effect on the gastrointestinal tract. Fatigue is also a common symptom, as the body's immune response to excess histamine can be draining.
Factors Contributing to High Histamine Levels
Several factors can contribute to high histamine levels in the body. Enzyme deficiencies, such as reduced activity of diamine oxidase (DAO) or histamine N-methyltransferase (HNMT), can impair the breakdown of histamine, leading to an accumulation. DAO is responsible for breaking down histamine in the gut, while HNMT breaks it down in other tissues.
In addition to enzyme deficiencies, the presence of certain gut disorders can worsen histamine intolerance. Leaky gut syndrome, for example, refers to increased intestinal permeability, allowing larger molecules, including histamine, to pass through the gut barrier and enter the bloodstream. This can lead to higher histamine levels in the body. Small intestinal bacterial overgrowth (SIBO) is another condition that can contribute to histamine intolerance, as certain bacteria in the small intestine produce histamine.
Understanding the factors contributing to high histamine levels is crucial in developing personalized treatment strategies for individuals with histamine intolerance. By addressing these underlying causes, it is possible to effectively manage the condition and improve overall well-being.
Recognizing the Symptoms of Histamine Intolerance
Histamine intolerance is a condition that occurs when there is an excessive buildup of histamine in the body. This can happen when the body is unable to break down histamine properly or when there is an overproduction of histamine. Recognizing the symptoms of histamine intolerance is crucial in managing the condition effectively.
Common symptoms of histamine intolerance include headaches, migraines, nasal congestion, sneezing, itching, hives, digestive issues such as diarrhea or abdominal pain, and even anxiety or panic attacks. These symptoms can vary in severity and may occur shortly after consuming high-histamine foods or being exposed to other triggers.
Foods to Avoid for Histamine Intolerance
For individuals with histamine intolerance, avoiding or reducing the consumption of high-histamine foods is crucial in managing symptoms. This includes foods like aged cheeses, cured meats, fermented foods, and alcoholic beverages. These foods are known to contain high levels of histamine and can trigger symptoms in sensitive individuals.
Additionally, certain foods can liberate histamine from mast cells, exacerbating symptoms. These include citrus fruits, tomatoes, and spinach. While these foods may be considered healthy choices for most people, individuals with histamine intolerance may need to limit or avoid them to prevent symptom flare-ups.
Working with a healthcare professional or registered dietitian can help create an individualized plan to identify trigger foods and make appropriate dietary modifications. They can also provide guidance on alternative food choices that are lower in histamine.
Managing Histamine Intolerance: Treatment Options
There is no cure for histamine intolerance, but management revolves around reducing histamine levels and avoiding triggers. Antihistamine medications can help alleviate symptoms in the short term, but lifestyle modifications are typically necessary for long-term management.
Lifestyle modifications may include dietary changes, stress reduction techniques, and lifestyle adjustments. By identifying and avoiding trigger foods, individuals can prevent symptom flare-ups. Stress reduction techniques such as meditation, yoga, or deep breathing exercises can help manage stress, which can worsen symptoms in some individuals. Making lifestyle adjustments, such as getting enough sleep and regular exercise, can also contribute to overall well-being and symptom management.
Testing for Histamine Intolerance: Is It Possible?
While there is no definitive test for histamine intolerance, several approaches can help in diagnosis. These include a detailed medical history, elimination diets, and measuring DAO enzyme activity.
A detailed medical history can provide valuable insights into a person's symptoms and potential triggers. Elimination diets involve removing high-histamine foods from the diet for a period of time and then reintroducing them to observe any changes in symptoms. Measuring DAO enzyme activity can help determine if there is a deficiency in the enzyme responsible for breaking down histamine.
However, it is essential to work with a healthcare professional to ensure an accurate diagnosis, as histamine intolerance can often be confused with other conditions. They can guide individuals through the diagnostic process and help create an appropriate treatment plan.
Strategies for Managing and Treating Histamine Intolerance
Managing histamine intolerance involves a multifaceted approach. Strategies may include identifying and avoiding triggers, supporting histamine breakdown with supplements, addressing any underlying gut disorders, and reducing stress levels.
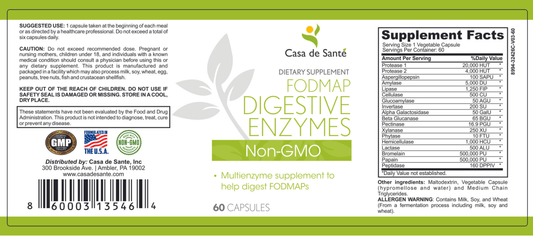
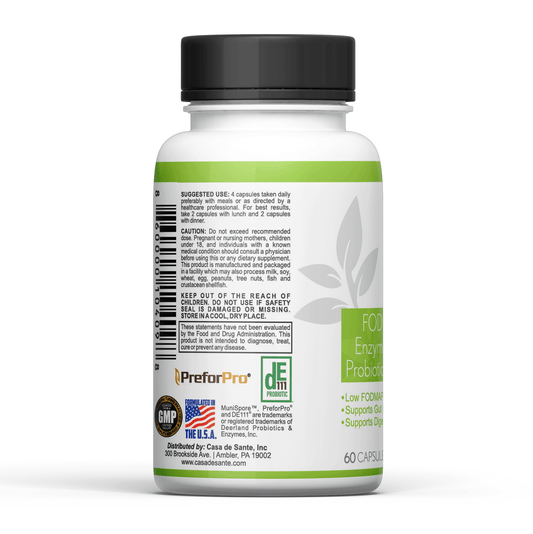
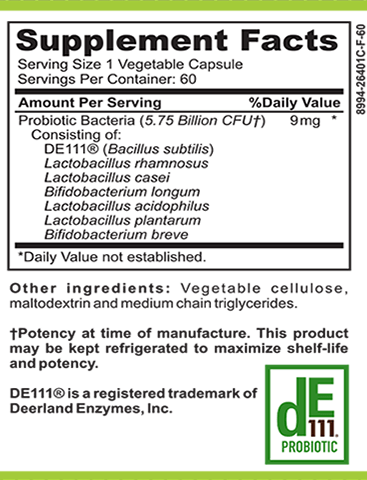
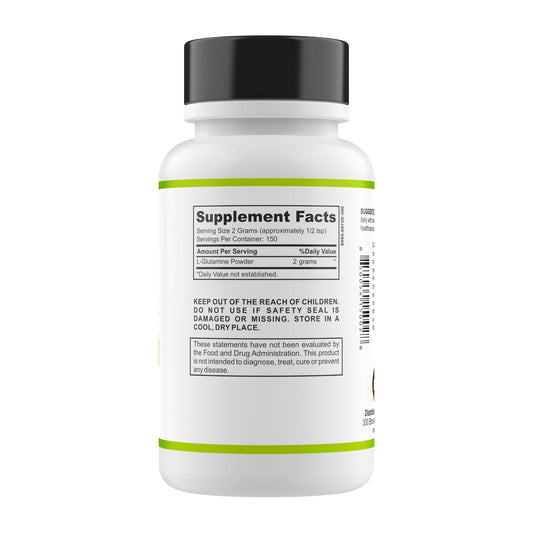
Identifying and avoiding triggers is crucial in preventing symptom flare-ups. This may involve keeping a food diary to track symptoms and identify potential trigger foods. Supporting histamine breakdown can be achieved through the use of supplements such as DAO (diamine oxidase) or vitamin C, which can help enhance the body's ability to break down histamine.
Addressing any underlying gut disorders, such as leaky gut syndrome or small intestinal bacterial overgrowth (SIBO), can also be beneficial in managing histamine intolerance. These conditions can contribute to increased histamine levels in the body. Working with a healthcare professional experienced in gut health can help identify and address these underlying issues.
Reducing stress levels is another important aspect of managing histamine intolerance. Stress can trigger histamine release and worsen symptoms. Incorporating stress reduction techniques such as mindfulness meditation, regular exercise, and sufficient sleep into daily routines can help manage stress and improve overall well-being.
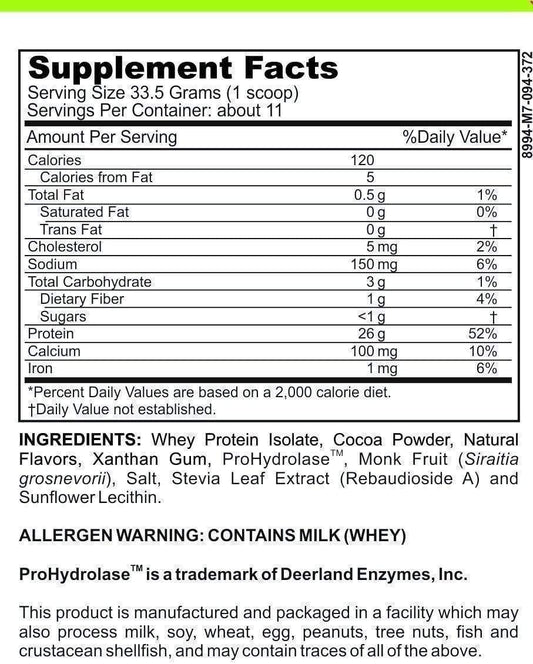
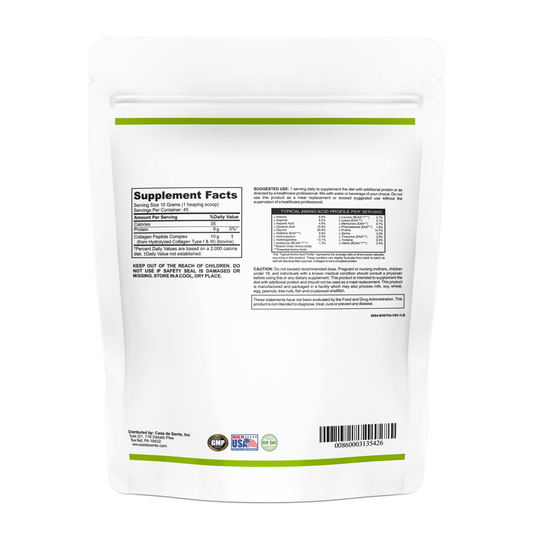
Additionally, maintaining a balanced and nutrient-rich diet can help support overall histamine regulation in the body. Consuming a variety of fresh fruits, vegetables, lean proteins, and healthy fats can provide the body with essential nutrients and support optimal functioning.
Consulting with a healthcare professional experienced in histamine intolerance management is crucial for creating an effective treatment plan. They can provide personalized guidance and support to help individuals manage their symptoms and improve their quality of life.
Understanding the causes, symptoms, and management options for histamine intolerance is essential for those affected by this condition. By gaining insights into the underlying processes and triggers, individuals can take proactive steps towards improving their quality of life and finding relief from the symptoms associated with histamine intolerance.