The Impact of Stress on Histamine Intolerance: Exploring the Toxic Relationship
In recent years, there has been a growing interest in the relationship between stress and histamine intolerance. Histamine intolerance is a condition where individuals experience adverse reactions to foods high in histamine due to their body's inability to properly break down and metabolize this compound. While the underlying causes of histamine intolerance are still not fully understood, stress has been identified as a significant factor that can exacerbate symptoms and contribute to the development of this condition.
Understanding Histamine Intolerance
Before delving into the impact of stress on histamine intolerance, it's crucial to grasp the basics of this condition. Histamine intolerance is often misunderstood and misdiagnosed due to its wide range of symptoms that can mimic other disorders. Individuals with histamine intolerance may experience symptoms such as headaches, flushing of the skin, hives, digestive issues, and respiratory problems.
Unraveling the mystery behind histamine intolerance requires an understanding of how histamine functions in the body. Histamine is a natural chemical involved in various physiological processes, including regulating immune responses and stomach acid production. In a healthy individual, the body produces sufficient amounts of enzymes, such as diamine oxidase (DAO), to break down and metabolize histamine. However, in individuals with histamine intolerance, this process is impaired.
One of the key factors contributing to the development of histamine intolerance is genetics. Research has shown that certain genetic variations can lead to reduced production of DAO, the enzyme responsible for breaking down histamine. This genetic predisposition can make individuals more susceptible to histamine intolerance and its associated symptoms.
Gut health imbalances also play a significant role in the development of histamine intolerance. The gut is home to trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in maintaining overall health. Imbalances in the gut microbiota, such as an overgrowth of certain bacteria or a lack of diversity, can disrupt the normal breakdown of histamine in the gut. This can lead to an accumulation of histamine in the body and trigger symptoms of histamine intolerance.
In addition to genetics and gut health, certain medications can also contribute to histamine intolerance. Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, can interfere with the normal breakdown of histamine in the body. This can exacerbate symptoms in individuals with histamine intolerance or even trigger histamine intolerance in individuals who were previously asymptomatic.
Furthermore, dietary habits can play a significant role in histamine intolerance. Histamine is naturally present in various foods, such as aged cheeses, fermented foods, and cured meats. For individuals with histamine intolerance, consuming these histamine-rich foods can lead to an accumulation of histamine in the body and trigger symptoms. Additionally, certain foods, such as citrus fruits, tomatoes, and alcohol, can stimulate the release of histamine in the body, further exacerbating symptoms.
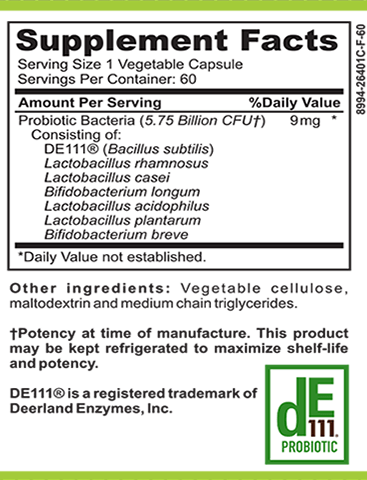
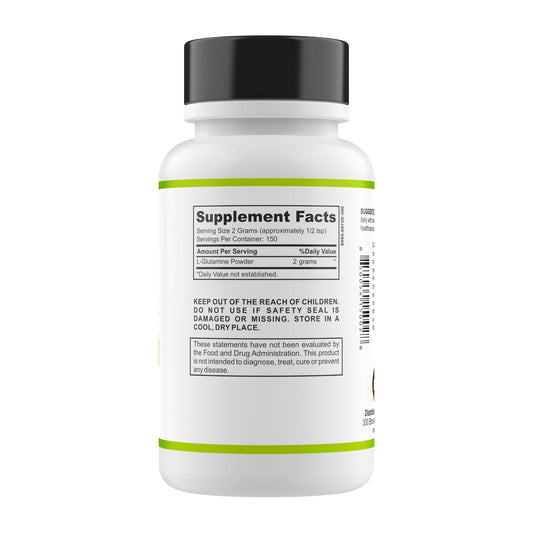
Managing histamine intolerance involves identifying and addressing these contributing factors. Genetic testing can help individuals understand their genetic predisposition to reduced DAO production and guide personalized treatment plans. Restoring gut health through dietary changes, probiotic supplementation, and addressing any underlying gut imbalances can also be beneficial. Avoiding histamine-rich foods and identifying individual triggers can help individuals minimize symptom flare-ups and improve their overall well-being.
The Connection Between Histamine and Stress
Stress, both acute and chronic, has a profound impact on our body's intricate systems. It affects hormone levels, immune responses, and neurotransmitter function ��� all of which can influence histamine intolerance.
Exploring the link between histamine and stress uncovers a complex relationship. Stress can trigger the release of histamine in the body, leading to symptoms in individuals with histamine intolerance. Additionally, stress may impair DAO enzyme activity, worsening histamine intolerance symptoms.
The impact of histamine intolerance on mental health is another area that deserves attention. Individuals with histamine intolerance may be more susceptible to anxiety, depression, and other mood disorders. The constant battle between stress and histamine intolerance can create a vicious cycle, as stress exacerbates symptoms, and the symptoms, in turn, contribute to additional stress.
Moreover, the effects of histamine intolerance on sleep should not be disregarded. Histamine plays a role in regulating wakefulness and sleep, and disturbances in histamine levels can lead to insomnia and poor sleep quality. This, in turn, further increases stress levels, creating a detrimental cycle of sleep deprivation and histamine intolerance symptoms.
Managing panic attacks in individuals with histamine intolerance also poses unique challenges. Panic attacks can be triggered by increased histamine levels, leading to intense fear and discomfort. Recognizing these connections and addressing the root causes can empower individuals with histamine intolerance to regain control over their mental and emotional well-being.
Furthermore, it is important to understand the impact of stress on histamine levels. When the body experiences stress, it releases stress hormones such as cortisol. These hormones can stimulate the release of histamine, leading to an increase in histamine levels. For individuals with histamine intolerance, this can result in a range of symptoms including headaches, nasal congestion, hives, and digestive issues.
Additionally, stress can also impair the activity of the enzyme diamine oxidase (DAO), which is responsible for breaking down histamine in the body. When DAO activity is compromised, histamine levels can build up, exacerbating symptoms of histamine intolerance. This can create a challenging situation for individuals as stress not only triggers the release of histamine but also impairs the body's ability to break it down effectively.
Moreover, the impact of histamine intolerance on mental health cannot be overlooked. Research has shown that individuals with histamine intolerance may be more prone to anxiety, depression, and other mood disorders. The constant battle between stress and histamine intolerance can create a vicious cycle, where stress worsens histamine intolerance symptoms, and the symptoms, in turn, contribute to additional stress. This interplay between stress and histamine intolerance can have a profound effect on an individual's overall well-being.
Furthermore, histamine also plays a crucial role in regulating sleep-wake cycles. Histamine is involved in promoting wakefulness, and disruptions in histamine levels can lead to sleep disturbances. For individuals with histamine intolerance, this can result in difficulties falling asleep, staying asleep, and overall poor sleep quality. The lack of restful sleep can further increase stress levels, creating a detrimental cycle where sleep deprivation worsens histamine intolerance symptoms and increased histamine levels contribute to poor sleep.
Lastly, managing panic attacks in individuals with histamine intolerance presents unique challenges. Panic attacks can be triggered by increased histamine levels, leading to intense fear, palpitations, shortness of breath, and a sense of impending doom. Recognizing the connection between histamine and panic attacks is crucial in providing effective support and treatment for individuals with histamine intolerance. By addressing the root causes and implementing strategies to manage histamine levels and stress, individuals can regain control over their mental and emotional well-being.
Strategies to Reduce Histamine and Stress
There are various approaches to reduce histamine and stress levels, enabling individuals to better manage their histamine intolerance symptoms and enhance their overall quality of life.
Living with histamine intolerance can be challenging, but with the right strategies, it is possible to find relief. In addition to the lifestyle changes and dietary approaches mentioned above, there are other techniques that can help individuals cope with histamine intolerance and reduce stress levels.
Lifestyle Changes to Combat Histamine Intolerance
Lifestyle modifications can play a significant role in mitigating histamine intolerance symptoms. Engaging in regular exercise not only helps to reduce stress but also improves overall well-being. Physical activity releases endorphins, which are natural mood boosters, and helps to promote a sense of calm and relaxation.
Practicing stress-management techniques such as mindfulness and yoga can also be beneficial. Mindfulness involves being fully present in the moment and paying attention to thoughts, feelings, and sensations without judgment. This practice can help individuals become more aware of their body's reactions to histamine and stress, allowing them to respond in a more mindful and balanced way.
Ensuring adequate sleep is another crucial aspect of managing histamine intolerance. Sleep deprivation can increase stress levels and exacerbate symptoms. Creating a relaxing bedtime routine, avoiding electronic devices before bed, and creating a comfortable sleep environment can all contribute to better sleep quality.
It is also important to identify and address any underlying gut health imbalances and food sensitivities. The gut plays a significant role in histamine metabolism, so optimizing gut health can help reduce histamine levels. Working with a healthcare professional to implement a comprehensive gut healing protocol can restore balance to the digestive system and minimize the impact of histamine intolerance on overall well-being.
Dietary Approaches for Managing Histamine Intolerance
Adopting a low-histamine diet is a common strategy for managing histamine intolerance. This involves avoiding or limiting the consumption of foods high in histamine, such as aged cheeses, cured meats, fermented foods, and alcohol. Additionally, certain foods, such as citrus fruits and tomatoes, can stimulate the release of histamine in the body and may need to be limited.
Incorporating foods that support the breakdown and elimination of histamine can also be beneficial. Foods rich in vitamin C, such as bell peppers, strawberries, and kiwi, have been shown to have anti-histamine properties. Quercetin, found in foods like onions, apples, and broccoli, can also help reduce histamine levels in the body. Including these foods in the diet can provide additional support in managing histamine intolerance.
Experimenting with an elimination diet under the guidance of a healthcare professional can help individuals identify triggers and develop a personalized dietary plan. This process involves temporarily removing potential trigger foods from the diet and gradually reintroducing them to determine which ones may be contributing to symptoms. Keeping a food diary can also be helpful in tracking symptoms and identifying patterns.
Stress-Relief Techniques for Histamine Intolerance
Reducing stress levels is crucial for individuals with histamine intolerance. Stress can trigger histamine release in the body, leading to increased symptoms. Engaging in activities such as meditation, deep breathing exercises, and aromatherapy can help promote relaxation and alleviate stress. These techniques help activate the body's relaxation response, reducing the production of stress hormones and calming the nervous system.
Additionally, seeking support from a mental health professional or joining support groups can provide individuals with valuable coping strategies and emotional support. Histamine intolerance can be overwhelming, and having a supportive network can make a significant difference in managing stress and improving overall well-being.
Remember, managing histamine intolerance and reducing stress is a journey that requires patience and self-care. By implementing these strategies and finding what works best for you, it is possible to find relief and improve your quality of life.
Addressing the Root Cause of Histamine Intolerance
While managing symptoms is essential, addressing the root cause of histamine intolerance is paramount to achieving long-term relief. Working with a healthcare professional who specializes in integrative and functional medicine can help identify and address the underlying factors contributing to histamine intolerance, such as gut dysbiosis, nutrient deficiencies, or genetic mutations.
By implementing personalized treatment plans that target the root cause, individuals can not only reduce their histamine intolerance symptoms but also improve their overall health and well-being.
Overall, recognizing the impact of stress on histamine intolerance is crucial for those affected by this condition. Understanding the intricate relationship between stress, histamine, and its effects on mental health, sleep, and panic attacks can guide individuals in making informed decisions to manage their symptoms effectively. By implementing lifestyle changes, adopting a low-histamine diet, and utilizing stress-relief techniques, individuals can regain control of their health and experience relief from the burdens of histamine intolerance.