Is IBS The Same As Dyspepsia
IBS (Irritable Bowel Syndrome) and dyspepsia, often referred to as indigestion, are two conditions that can cause gastrointestinal discomfort and disrupt one's quality of life. While both conditions share similarities in terms of symptoms and treatment, they are not the same. In this article, we will explore the characteristics of IBS and dyspepsia, compare their differences, discuss diagnosis and treatment options, and provide guidance on living with these conditions.
Understanding IBS and Dyspepsia
Welcome to our comprehensive guide on understanding IBS (Irritable Bowel Syndrome) and dyspepsia. In this article, we will delve into the definitions, symptoms, and causes of these two common digestive disorders.
Defining IBS: Symptoms and Causes
IBS, also known as Irritable Bowel Syndrome, is a chronic disorder that primarily affects the large intestine. Individuals with IBS often experience a range of distressing symptoms, including abdominal pain, bloating, excessive gas, diarrhea, and constipation.
The exact cause of IBS remains unknown, but medical experts believe that it involves a combination of factors. These factors may include abnormal muscle contractions in the intestine, increased sensitivity of the gut, and changes in the gut microbiota, which refers to the complex community of microorganisms residing in our digestive system.
It is important to note that IBS is a highly individualized condition, with symptoms varying in intensity and duration from person to person. Some individuals may experience mild symptoms that are easily manageable, while others may face more severe and debilitating symptoms.
Furthermore, individuals with IBS often report experiencing flare-ups, which are episodes of heightened symptoms. These flare-ups can be triggered by various factors, including stress, certain foods, hormonal changes, or other environmental factors. Understanding and identifying these triggers can be crucial in managing and reducing the frequency of flare-ups.
Defining Dyspepsia: Symptoms and Causes
Dyspepsia, commonly referred to as indigestion, is a term used to describe a range of symptoms related to the upper digestive tract. These symptoms may include pain or discomfort in the upper abdomen, bloating, feeling full quickly when eating, and nausea.
There are several factors that can contribute to the development of dyspepsia. Overeating and eating too quickly are common culprits, as they can put excessive strain on the digestive system. Consuming fatty or spicy foods, smoking, and alcohol consumption are also known to trigger dyspeptic symptoms.
It is important to note that dyspepsia can be either occasional or frequent, depending on the underlying causes and individual circumstances. In some cases, dyspepsia may be a symptom of an underlying condition, such as gastroesophageal reflux disease (GERD) or peptic ulcers. Therefore, it is crucial to consult a healthcare professional for a proper evaluation and diagnosis.
In conclusion, IBS and dyspepsia are two common digestive disorders that can significantly impact an individual's quality of life. While the exact causes of these conditions are still being researched, understanding the symptoms and triggers can help individuals better manage their symptoms and seek appropriate medical guidance when necessary.
Comparing IBS and Dyspepsia
Similarities Between IBS and Dyspepsia
Both IBS and dyspepsia affect the digestive system and can cause discomfort or pain in the abdominal area. They can both be triggered or worsened by certain foods, stress, or other environmental factors. Furthermore, both conditions can significantly impact an individual's daily life, leading to reduced quality of life and emotional distress.
Individuals who suffer from both IBS and dyspepsia may find themselves facing a double burden. The coexistence of these two conditions can complicate the management of symptoms, as the triggers and treatment options for each may differ. It becomes crucial for individuals to work closely with their healthcare providers to develop a personalized management plan that addresses both conditions simultaneously.
Moreover, the impact of IBS and dyspepsia extends beyond the physical symptoms. The emotional toll of living with chronic digestive disorders cannot be overlooked. The constant discomfort, unpredictable symptoms, and limitations on daily activities can lead to increased stress, anxiety, and even depression. It is essential for individuals to seek emotional support and explore coping mechanisms to navigate the challenges posed by these conditions.
Differences Between IBS and Dyspepsia
While IBS primarily affects the large intestine, dyspepsia is centered around symptoms related to the upper digestive tract. The specific symptoms experienced are also different. For instance, IBS is commonly associated with changes in bowel habits, such as alternating episodes of diarrhea and constipation, while dyspepsia may include symptoms such as heartburn or acid reflux.
Understanding the underlying causes of IBS and dyspepsia can shed light on their differences. IBS is thought to involve a combination of factors, including abnormalities in intestinal muscle contractions and increased gut sensitivity. This complex interplay of factors can lead to the characteristic symptoms experienced by individuals with IBS.
On the other hand, dyspepsia may be caused by lifestyle factors, underlying gastrointestinal conditions, or inflammation of the stomach lining. Factors such as excessive alcohol consumption, smoking, or certain medications can contribute to the development of dyspepsia. In some cases, dyspepsia may be a symptom of an underlying condition, such as gastroesophageal reflux disease (GERD) or peptic ulcers.
It is important to note that while IBS and dyspepsia have distinct characteristics, there can be overlap in symptoms. This overlap can make diagnosis and treatment challenging, as healthcare providers need to carefully evaluate the individual's medical history, symptoms, and conduct appropriate diagnostic tests to differentiate between the two conditions.
In conclusion, while IBS and dyspepsia share certain similarities in terms of their impact on the digestive system and quality of life, they also have distinct differences in terms of the affected areas of the digestive tract and specific symptoms experienced. Understanding these similarities and differences is crucial for individuals and healthcare providers alike to effectively manage and treat these chronic digestive disorders.
Diagnosis and Treatment
How IBS is Diagnosed
Diagnosing Irritable Bowel Syndrome (IBS) involves a thorough evaluation of symptoms, medical history, and physical examination. The healthcare professional will take into account the patient's reported symptoms, such as abdominal pain, bloating, and changes in bowel habits. They will also inquire about the frequency and duration of these symptoms.
Additional tests may be ordered to rule out other conditions with similar symptoms. Stool analysis can help identify any abnormalities or infections in the gastrointestinal tract. Blood tests may be conducted to check for signs of inflammation or to rule out other conditions. Imaging studies, such as an abdominal ultrasound or a CT scan, may also be recommended to visualize the digestive organs and identify any structural abnormalities.
The Rome criteria, a set of guidelines developed by experts in the field, are commonly used to aid in the diagnosis of IBS. These criteria help healthcare professionals categorize the patient's symptoms and determine if they meet the criteria for a diagnosis of IBS.
Once a diagnosis of IBS is confirmed, treatment is typically focused on symptom management. This can involve a combination of dietary modifications, stress reduction techniques, medication, and lifestyle changes.
How Dyspepsia is Diagnosed
The diagnosis of dyspepsia usually begins with a thorough medical history and physical examination. The healthcare professional will ask the patient about their symptoms, such as upper abdominal pain, bloating, and early satiety. They will also inquire about any factors that may trigger or worsen these symptoms, such as certain foods or stress.
Depending on the suspected cause, additional tests may be conducted to further evaluate the patient's condition. Blood tests can help identify any underlying infections or abnormalities in organ function. An upper endoscopy, where a flexible tube with a camera is inserted through the mouth to visualize the upper digestive tract, may be performed to examine the lining of the esophagus, stomach, and duodenum. Imaging studies, such as an abdominal ultrasound or a CT scan, may also be recommended to assess the structure and function of the digestive organs.
Once a diagnosis of dyspepsia is made, treatment depends on the underlying cause. Lifestyle modifications are often recommended as a first-line approach. This can include dietary changes, such as avoiding trigger foods or adopting a more balanced diet. Weight management and stress reduction techniques, such as regular exercise and relaxation exercises, can also help alleviate symptoms.
Medications may be prescribed to alleviate symptoms and manage the underlying cause. Antacids can help neutralize stomach acid and provide temporary relief from heartburn or acid reflux. Acid blockers, such as proton pump inhibitors or H2 blockers, can reduce the production of stomach acid and alleviate symptoms. Prokinetics may be prescribed to improve gastric emptying and reduce symptoms of bloating and early satiety. In cases where dyspepsia is a symptom of an underlying condition, treating the primary cause may be necessary to alleviate symptoms.
Treatment Options for IBS
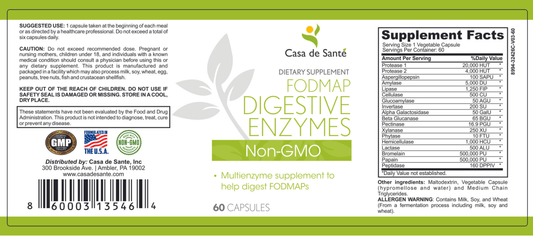
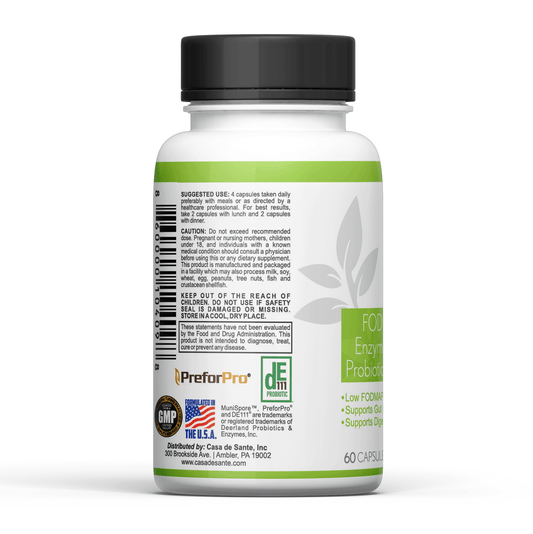
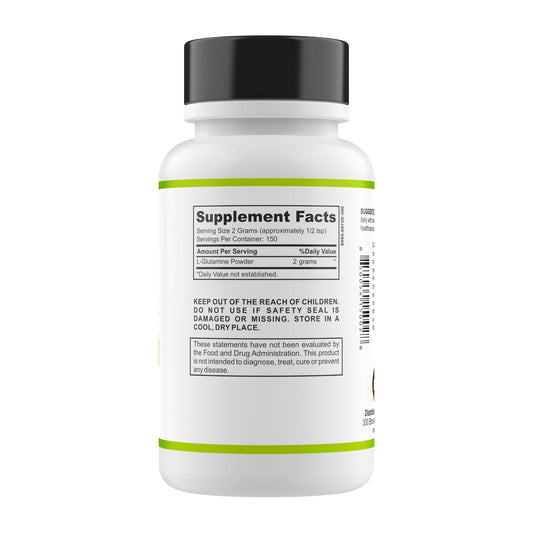
Managing IBS involves a multidimensional approach tailored to the individual patient. Dietary adjustments can play a significant role in symptom management. Identifying and avoiding trigger foods, such as those high in fat, caffeine, or artificial sweeteners, can help alleviate symptoms. Some individuals may benefit from following a low FODMAP diet, which restricts certain carbohydrates that can trigger IBS symptoms.
Stress reduction techniques can also provide relief for individuals with IBS. Relaxation exercises, such as deep breathing or meditation, can help calm the nervous system and reduce symptoms. Cognitive-behavioral therapy or counseling may be recommended to address any underlying psychological factors contributing to IBS symptoms.
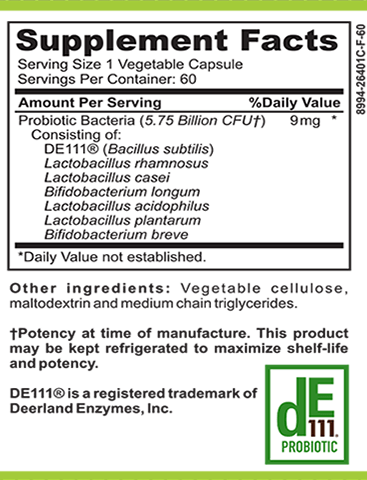
In addition to lifestyle modifications, medications may be prescribed to control specific symptoms. Antispasmodic drugs can help reduce intestinal cramps and relieve abdominal pain. Laxatives or antidiarrheal medications may be used to regulate bowel movements and manage diarrhea or constipation. Probiotics, which are beneficial bacteria, may be recommended to restore the balance of gut flora and improve digestive function.
It is important for individuals with IBS to work closely with a healthcare professional to develop an individualized treatment plan. Regular follow-up appointments can help monitor symptoms and make any necessary adjustments to the treatment plan.
Treatment Options for Dyspepsia
The treatment of dyspepsia depends on the underlying cause and may involve a combination of lifestyle modifications and medications. Avoiding trigger foods is often recommended to alleviate symptoms. This can include reducing the intake of spicy or fatty foods, as well as avoiding excessive alcohol consumption or smoking.
Maintaining a healthy weight is also important for individuals with dyspepsia. Excess weight can put pressure on the stomach, leading to symptoms of heartburn or acid reflux. Weight management strategies, such as regular exercise and portion control, can help alleviate symptoms.
Stress management techniques can play a significant role in managing dyspepsia symptoms. Engaging in relaxation exercises, such as yoga or deep breathing, can help reduce stress levels and alleviate symptoms. Seeking support from a therapist or counselor can also be beneficial in addressing any underlying psychological factors contributing to dyspepsia.
Medications may be prescribed to alleviate symptoms and manage the underlying cause of dyspepsia. Antacids can provide temporary relief from heartburn or acid reflux by neutralizing stomach acid. Acid blockers, such as proton pump inhibitors or H2 blockers, can reduce the production of stomach acid and alleviate symptoms. Prokinetics may be prescribed to improve gastric emptying and reduce symptoms of bloating and early satiety.
In cases where dyspepsia is a symptom of an underlying condition, treating the primary cause may be necessary to alleviate symptoms. This may involve additional medications or interventions specific to the underlying condition.
Living with IBS and Dyspepsia
Lifestyle Changes for Managing IBS
Living with IBS can be challenging, but certain lifestyle changes can help manage symptoms. Regular exercise, getting enough sleep, and practicing stress-reducing techniques, such as yoga or meditation, can contribute to symptom relief. Maintaining a balanced diet and staying hydrated are also important.
Support groups or counseling can provide guidance and emotional support for individuals with IBS. In some cases, cognitive-behavioral therapy may be beneficial in managing stress and improving coping mechanisms.
Lifestyle Changes for Managing Dyspepsia
Individuals with dyspepsia can adopt lifestyle changes to reduce symptoms. Eating smaller, more frequent meals, avoiding trigger foods, like fatty or spicy foods, and refraining from eating close to bedtime, are recommended.
Engaging in stress-reducing activities, such as regular exercise, mindfulness practices, or hobbies, can also contribute to managing dyspepsia. Maintaining a healthy weight and avoiding smoking and excessive alcohol consumption are additional lifestyle factors that can help minimize symptoms.
Conclusion: Are IBS and Dyspepsia the Same?
In conclusion, IBS and dyspepsia are separate conditions, albeit sharing some similarities. While they both affect the digestive system and can cause discomfort, their symptoms and causes differ. Accurate diagnosis is crucial for appropriate treatment strategies.
It is important to consult with a healthcare professional for an accurate diagnosis and individualized treatment plan. By understanding the unique characteristics of IBS and dyspepsia, individuals can take proactive steps towards managing their symptoms and improving their overall well-being.